From Stage 0 to 3: Injectable Induction Agents – New and Old
Odette O, DVM, DACVAA
Massachusetts Veterinary Referral Hospital, Woburn, MA
Posted on 2016-10-04
General anesthesia provides us with unconciousness, amnesia, analgesia, muscle relaxation, and the ability to perform various procedures in our veterinary patients. The use of injectable anesthetic agents allows us to get our patients from premeded-awake to surgical plane of anesthesia, while minimizing the use of inhalant anesthesia and its associated cardiovascular and respiratory depression. This allows us to perform a short procedure and/or place an endotracheal tube so that we can use inhalant anesthesia for a longer procedure or even provide supplemental oxygen for a short procedure. An ideal injectable anesthetic agent would be one that is rapidly acting, minimally dependent on metabolism for termination of effects, short-acting, water-soluble, non-irritating to tissues, inexpensive, stable in solution, with negligible negative effects on the cardiovascular and respiratory systems. Since such an agent does not exist yet in veterinary medicine, we are left to select an agent based on a number of factors based on the patient needs, safety, and logistics. Species, age, breed, current physical status, anticipated procedure time, availability of equipment & personnel, as well as familiarity with the technique are all considerations in making an induction plan.
Why use an induction agent?
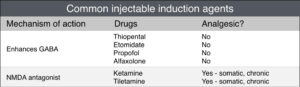 Use of an induction agent, especially with the background of having given pre-anesthetic medications (sedative + opioid) will decrease the amount of inhalant needed to achieve a surgical plane of anesthesia, thereby decreasing the cardiac and respiratory depressing effects of inhalant use alone. The use of injectable anesthetic agents for induction also helps to minimize the patient struggling that we may see when using just inhalant alone, since they smooth the transition from awake (0) to surgical anesthesia (3) in seconds instead of the minutes it would take when using inhalants alone. This minimizes patient stress and the associated catecholamine release. However, these drugs themselves can have important negative side effects, so the goal is also to use the minimum dose necessary in order to facilitate a safe induction. Knowing their main mechanism of action aids in understanding their effects as well as undesirable side effects (see table). The gamma-amino-butyric acid (GABA) enhancing drugs tend to have a rapid onset of action, good muscle relaxation, but also result in dose-related cardiovascular and respiratory depression with the potential for apnea. The N-methyl-D-aspartate (NMDA) antagonist drugs cause a dissociative anesthesia, with the potential for tachycardia and hypertension, as well as skeletal muscle rigidity when used without a muscle relaxant. For this reason, the dissociatives are often combined with a benzodiazepine. The onset of action for the NMDA antagonists is still rapid, but slightly longer than the GABA-enhancing drugs, about 60 seconds.
Use of an induction agent, especially with the background of having given pre-anesthetic medications (sedative + opioid) will decrease the amount of inhalant needed to achieve a surgical plane of anesthesia, thereby decreasing the cardiac and respiratory depressing effects of inhalant use alone. The use of injectable anesthetic agents for induction also helps to minimize the patient struggling that we may see when using just inhalant alone, since they smooth the transition from awake (0) to surgical anesthesia (3) in seconds instead of the minutes it would take when using inhalants alone. This minimizes patient stress and the associated catecholamine release. However, these drugs themselves can have important negative side effects, so the goal is also to use the minimum dose necessary in order to facilitate a safe induction. Knowing their main mechanism of action aids in understanding their effects as well as undesirable side effects (see table). The gamma-amino-butyric acid (GABA) enhancing drugs tend to have a rapid onset of action, good muscle relaxation, but also result in dose-related cardiovascular and respiratory depression with the potential for apnea. The N-methyl-D-aspartate (NMDA) antagonist drugs cause a dissociative anesthesia, with the potential for tachycardia and hypertension, as well as skeletal muscle rigidity when used without a muscle relaxant. For this reason, the dissociatives are often combined with a benzodiazepine. The onset of action for the NMDA antagonists is still rapid, but slightly longer than the GABA-enhancing drugs, about 60 seconds.
Barbiturates
The main clinically used barbiturate for anesthesia induction is/was thiopental. This drug is still available and widely used in other parts of the world, so it will get a brief mention here. Thiopental enhances GABA and is rapid-acting (20-30s) with a short duration of action (10-15 minutes). It is recommended that this drug be administered only through a well-placed IV catheter, as it is very alkaline and perivascular administration can lead to significant tissue sloughing. Dose-related respiratory depression leading to apnea can be seen with this drug, as well as decreased cardiac stroke volume and systemic vascular resistance leading to hypotension. Thiopental can be arrhythmogenic, so its use in patients with underlying cardiac disease should be avoided. Repeated boluses of this drug should be avoided, as prolonged recovery may result. In addition, this drug is not recommended in sight hounds, as they have a high muscle ratio and also an insufficient cytochrome P450 hydroxylation pathway.
Etomidate
Etomidate is a GABA-enhancing, short-acting (10 min) imidazole induction agent that causes minimal cardiovascular depression. Despite its cost, it is an excellent choice for patients with significant underlying cardiovascular disease or hemodynamic instability. This drug causes dose-related respiratory depression and apnea. Use of a pre-anesthetic medication is strongly recommended, as myoclonus as well as severe retching and vomiting is seen when this drug is given to non-sedate patients. Another important note on this drug is that it is contraindicated in Addisonian patients, as it causes adrenocortical suppression for 2-3 hours after a single administration. Etomidate is currently on the market in two different formulations, one with propylene glycol and the other with intralipid. Both formulations require IV administration. The propylene glycol can cause pain on injection as well as hemolysis in small patients.
Propofol & Propofol 28
Propofol and propofol 28 are probably THE most commonly used induction agent in veterinary medicine today. This GABA-enhancing alkyl-phenol compound has a rapid onset and short duration of action (20 min), and is relatively noncumulative, making it a desirable induction agent. Regular propofol contains no preservative, and should be discarded 6 hours after opening. Propofol 28 contains a benzyl alcohol preservative and has a shelf-life of 28 days (Note: not labelled for use in cats). The formulation of this drug with soybean oil, egg lecithin, and glycol can make it painful for injection (especially in an “old” catheter) and limit its administration to IV only. This induction agent causes dose-related respiratory depression and potential apnea along with hypotension. Cats that require multiple consecutive anesthesia episodes in a row should be induced with agents other than only propofol, since when used in cats repeatedly (>3d in a row), significant red blood cell oxidative injury can result, causing a Heinz body anemia.
Alfaxalone
The newest induction agent on the market is actually a re-formulation of an old one. This neurosteroid is a GABA-enhancing drug and has the benefit of rapid onset (20-30s), short duration of action, and a high therapeutic index (safety margin). Dose-related respiratory depression leading to apnea may result, as well as hypotension. However, some studies have found slightly less cardiovascular depression with the use of alfaxalone when compared to propofol. This drug is best administered IV in most patients, but it also has some utility via IM injection for fractious small patients.
Ketamine & Tiletamine
Of all the induction drugs we discussed here, this group is the only one that does NOT work through enhancing GABA at the GABAa receptor. Ketamine and tiletamine are known as dissociative anesthetics. Both drugs cause an anesthetic state induced via interrupting the ascending transmission from portions of the brain dealing with conscious and unconscious functions. As a result, physical restraint is facilitated and unlike the other induction agents, a generalized state of depression is not seen – making ketamine and tiletamine amongst the safest drugs we use in veterinary medicine. Ketamine is formulated on its own, but tiletamine is part of a proprietary formulation along with zolazepam, known as Telazol. Both of these formulations may be administered either IV or IM. Clinically we see quite a different profile with use of these induction agents. The onset of action of these drugs is about 60-90 seconds. A cataleptoid state is seen in the patient – eyes open and moving, swallowing reflexes intact, and increased skeletal muscle tone. The increased muscle tone may be offset by pairing induction with a benzodiazepine such as diazepam or midazolam. Ketamine and tiletamine are also the only induction agents discussed here that are known to provide analgesia. These drugs are N-methyl-D-aspartate (NMDA) antagonists, providing somatic (skin and skeletal muscle) analgesia as well as playing an important role in the treatment of wind-up and chronic pain relief. Note: these effects are short-acting and dose-related, so the use of a CRI after induction is recommended. Administration of dissociative anesthetics (ketamine and tiletamine) causes sympathomimetic effects – increased heart rate and blood pressure may be seen in patients. In addition, dissociatives may sensitize the heart to catecholamine-induced arrhythmias, so use of these agents in patients who may not tolerate tachycardia, hypertension, or have an underlying cardiac electrical disturbance (i.e. GDV with VPCs, etc) is not recommended.
Induction Adjuncts
Benzodiazepines and lidocaine are commonly used induction adjuncts. These drugs are not capable of anesthetic induction when used alone, but may be added to a protocol in order to decrease the amount of induction agent needed, or to confer some other added benefit.
The benzodiazepines are often used as an adjunct for ketamine, propofol, etomidate, and even alfaxalone inductions. The most commonly used injectable benzodiazepines in veterinary medicine are diazepam and midazolam. These drugs mediate GABA at the GABAa receptor and have the benefit of being an anti-convulsant, providing muscle relaxation, and decreasing induction agent required. Although this group of drugs results in highly unpredictable sedation or even excitement in young, healthy dogs and cats when used as a pre-anesthetic medication, it definitely has its place as part of the induction protocol in patients with underlying cardiovascular disease, as well as significant hepatic and/or renal disease. Diazepam is not water-soluble, so it is formulated with propylene glycol and alcohol. This formulation makes it precipitate when mixed with any drug other than ketamine. It should be administered IV only. Diazepam is light sensitive and binds to plastic, so should not be drawn up much ahead of the anticipated procedure time. Midazolam is a water-soluble formulation of drug that becomes lipid soluble at physiologic pH, making it useful for many routes of administration including IV, IM, IN. Zolazepam is a benzodiazepine formulated with tiletamine in the proprietary formulation known as Telazol. Of all drugs discussed in this lecture series, the benzodiazepines are the only ones given at induction that are reversible – flumazenil is a competitive, selective benzodiazepine antagonist.
Lidocaine is a sodium channel blocker that can be used locally, regionally, or systemically. The use of is drug IV at induction confers analgesia to the patient and also blunts laryngeal reflexes and decreases the requirement of induction agent needed to produce anesthesia.
Special Inductions
Mask or chamber inductions: Due to the large amount of inhalant needed to induce and intubate the patient, as well as environmental and staff exposure to waste gases, this method of induction is generally NOT recommended for canine and feline patients. Excessive cardiovascular and respiratory depression with the inability to monitor the patient for a period of time is of great concern. However, if mask or chamber induction is to be performed, it is recommended that the patient be generously sedated prior to this procedure in order to minimize the excitatory phase seen as well as patient physiological and behavioral stress.
Opioid-benzodiazepine inductions: This method of anesthetic induction is reserved for and is only successful in severely debilitated patients. Using only a pure-mu agonist opioid along with a benzodiazepine with no other injectable agent for induction has the benefits of minimal CV and respiratory depression, it provides pre-emptive analgesia, and both drugs are reversible if a major complication is to arise. The use of topical lidocaine in order to blunt laryngeal reflexes and facilitate endotracheal intubation is helpful. The most important factor in success of this anesthetic induction protocol is to select patient CAREFULLY.
In Summary
Keep in mind that nothing in anesthesia and analgesia is absolute, this is as much art as it is science! There may be multiple appropriate choices, especially if the patient is healthy. The main goal is to avoid specific contraindications when selecting a patient protocol whenever possible. Most anesthetic cases can be performed successfully at your practice with careful attention to detail in order to recognize potential areas of concern and consideration ahead of time, along with proper preparation and planning. In cases where specific work-up, monitoring, or post-procedure care is of concern – referral of a case to an Anesthesiologist may also be an option.
Further reading
- Grimm KA, Lamont LA, Tranquilli WJ, Greene SA, and Robertson SA (eds) Veterinary Anesthesia and Analgesia, The Fifth Edition of Lumb and Jones. Wiley Blackwell, 2015.
- Smith LJ (ed). Questions and Answers in Small Animal Anesthesia. Wiley Blackwell, 2016.
About the author
|