Non-invasive point-of-care monitors in ER/ICU and anesthesia
Stephen Cital RVT, SRA, RLAT, VTS-LAM
United Veterinary Specialty and Emergency, Oakland Zoo, San Francisco Zoo
Posted on 2017-02-21 in Emergency & Critical Care, Anesthesia & analgesia
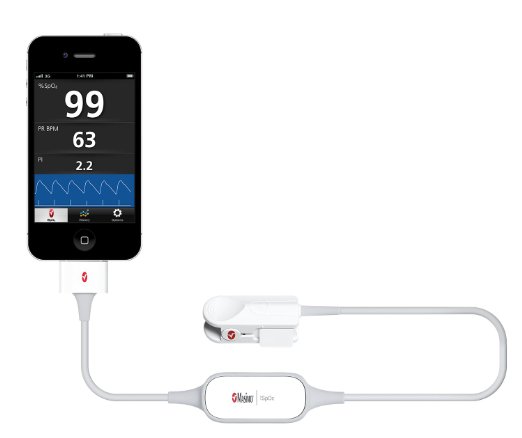
Technology, as we all know, is ever changing and advancing. Currently, there are iPhone® apps that read ECGs (AliveCor®), as well as phone applications designed to help diagnose arrhythmias. Then there is the launch of an SpO2 sensor attachment (iSpO2®, Masimo Corp.) that can be used as a personal SpO2 monitor for fitness, endurance and aviation training increases the number of portable point of care devices (Fig. 1).
Not all devices are marketed or have FDA approval for diagnostic use in the medical/veterinary setting.
I am focusing on one device in this blog, the Radical-7 Pulse CO-Oximeter (Fig. 2) by Masimo Corp. because it is the only FDA-approved non-invasive CO2-oximeter now being marketed for veterinary use. The technology does not necessarily have heaps of data for animal efficacy yet, but it is an important advancement that we as veterinary medical professionals should know is available. The utilization of the machine is gaining popularity in human medicine and now is the time for its utilization in veterinary medicine. Multiple human studies have found the individual components of the Masimo Radical-7® to be accurate within a reasonable margin of error for a point of care device.1,2
The use of standard pulse oximetry in veterinary medicine is widespread and a highly accepted form of non-invasive monitoring of oxygen saturation and pulse rate in critical, non-critical and anesthetized patients; the gold standard still being arterial blood gas sampling and EKG’s. Superior oxygen saturation and perfusion are essential in the ICU and OR for the best patient outcome and reduced healing times as well as normal organ function.1,3 Standard pulse oximeters use two wavelengths of light to calculate oxyhemoglobin, which is merely a total of hemoglobin, methemoglobin, carboxyhemoglobin, as well as other forms of possible dyshemoglobin’s that may be circulating. This combination is then expressed as a total percentage and displayed as the SpO2. The accepted reference interval for most species is 98-100%. With using the standard 2-wavelength pulse oximetry, it is easy to misinterpret SpO2% readings as “within normal limits” when a dyshemoglobin may be present.4
Can you remember the last time you ordered a dyshemoglobin profile or have ever had to treat one? Not only are dyshemoglobins under diagnosed in human medicine, but more so in veterinary medicine. Dyshemoglobins are caused by a metabolic disorder, toxin ingestion, toxin exposure or acquired from medications.1,2,4
Now you might be asking how dyshemoglobins are assessed? Invasive Co-oximeters have been around for a while in human medicine, but with little use in veterinary medicine. Invasive Co-Oximetry entails an actual blood sample running through a bench top Co-Oximetry machine.
However, the Masimo Radical-7 non-invasive Co-Oximetry only entails clipping or taping a regular looking SpO2 sensor to the patient. One might be asking how a SpO2 sensor will differentiate the different types of hemoglobins? The answer being the advanced non-invasive Co-Oximeter uses >7 wavelengths of infrared light to calculate a combined oxyhemoglobin reading as a total SpO2% and do to the increased sensitivity from the extra wavelengths of infrared light it also calculates and shows readings for two dyshemoglobins, methemoglobin and carboxyhemoglobin. The percentages of the two dyshemoglobins are then displayed as percentages on the screen. In our use of the machine, we discovered detectable levels of methemoglobin on the Radical-7, confirming with invasive Co-Oximetry. This was startling and an important discovery as it allowed us to change our anesthesia protocols to minimize acquired MetHb buildup for better patient care.
The standard hemoglobin reading the machine also can be very useful for animals undergoing blood transfusions. The machine, in addition, gives a total arterial oxygen content reading for further non-invasive monitoring. This parameter is excellent for ventilator cases or respiratory compromised patients.
Cardiovascular perfusion and balanced fluid therapy is yet another fundamental part of traditional patient monitoring using subjective opinion or complicated machinery. Advanced techniques to monitor such parameters can involve placing a central line for central venous pressure measurement or even placing and maintaining an arterial catheter. As we all know this may be difficult and not practical for the duration of a case or feasible in a certain species. Not to mention financially burdensome to the client or out of the scope of your practice’s needs and abilities. This, in turn, can lead to less effective treatment and response in our patients. The Masimo Radical-7 includes the features of Perfusion Index (PI) and Pleth-Variability Index (PVI). These are two newer monitoring parameters and can be very telling when obtained correctly. The perfusion index is the ratio of the pulsatile blood flow to the non-pulsatile or static blood in peripheral tissues. What this means is now we can monitor peripheral tissue perfusion in our patients non-invasively giving better insight into our fluid therapy management, cardiac/renal output, and efficacy of medications. A defined reference variable is not yet established in the canine or feline patient or any other species for that matter, other than humans, which tends to be quite broad. However, the PI parameter, as well as all of the other non-conventional parameters, is great for trending and monitoring. The PI is also a great tool for assessing the efficacy of opioids and epidurals. When full onset of the opioid or epidural occurs, we see a spike in the PI showing via vasodilation.
The Pleth Variability Index (PVI) is a new technology even in human medicine. It is a measurement of the change of perfusion index with a complete respiratory cycle. With this in mind, PVI is most reliable with patients undergoing mechanical ventilation. In a scientific abstract presented at the American College of Veterinary Anesthesiologists conference, one research group found that the PVI had a good correlation in detecting hypovolemia and return to normovolemia in dogs, but could not be used in definitively stating hypervolemia. Several more recent veterinary papers on PVI have come out with positive conclusions as to the reliability of predicting fluid responsiveness using this non-invasive tool.
The last parameter is the acoustic respiratory monitor. What this acoustic respiratory rate (aRR) monitor has to offer is continuous respiration monitoring without endotracheal tube placement. It is perfect for the ICU setting, especially with quiet or recumbent patients. It is also ideal for field procedures of large or exotic animals. The readings of the aRR on the Radical-7 have been nearly identical to our intubated patients when compared to the use of a traditional respirometer.
In all, the Masimo Radical-7 offers an all-inclusive and advanced monitoring device. It has brought attention to parameters never monitored before as well as reminding us of the importance of drug selection. Formal validating studies are underway with the Masimo Radical-7 for the veterinary community, and we anticipate positive results.
Further reading
- Shamir M., Avramich A., Smaka T. The Current Status of Continuous Noninvasive Measurement of Total, Carboxy, and Methemoglobin Concentration. International Anesthesia Research Society 2012; vol. 114(5): 972-978.
- Macket M, Allard M., Applegate R., Rook L. The Accuracy of noninvasive and Continuous Total Hemoglbin Measurment by Pulse CO-Oximetry in Human Subjects Undergoing Hemodilution. International Anesthesia Research Society 2010; vol. 111(6): 1424-1426.
- Erhardt W., Lendl R., Hipp G., et al. The use of pulse oximetry in clinical veterinary anaesthesia. Journal of the Association of Veterinary Anesthesiology 1990; 17: 30-31.
- Zaouter C., Zavorsky G. The measurement of carboxyhemoglobin and methemogloin using a non-invasive pulse Co-oximeter. Respiratory Physiology & Neurobiology 2012; 182:88-92.
- Masimo Radical-7 Operator Manual Masimo Corp. 2010.
- Ash-Bernal R., Wise R., Wright S. Acquired Methemoglobinemia: A Retrospective Series of 138 Cases at 2 Teaching Hospitals.Medicine 2004; 83: 265-272.
- Marik P., Monnet X., Teboul JL. Hemodynamic parameters to guide fluid therapy. Annals of Intensive Care 2011, 1:1.
- Cannesson M., Delannoy B., Morand A., et al. Does the Pleth Variablity Index Indicate the Respiratory Induced Variation in the Plethysmogram and Arterial Pressure Waveforms?. International Anesthesia Research Society 2008; vol. 106(4): 1189-1194.
About the authorStephen originally started college to become a Registered Nurse, but did not enjoy working with humans as patients. Instead, Stephen became an RVT and then obtained certification as a Surgical Research Anesthetist through the Academy of Surgical Research followed the designation of a Registered Laboratory Animal Technician through the American Association of Laboratory Animal Science soon after. Stephen is Executive Director for the Academy of Laboratory Animal Veterinary Technicians and Nurses which recently received Veterinary Technician Specialty status from NAVTA. His regular daytime position is in the surgery department and provides training at United Veterinary Specialty and Emergency, as well as a private contractor for several research organizations. Stephen also holds positions at the Oakland Zoo and the San Francisco Zoo. He occupies his remaining time writing book chapters, book reviews, blogs for VetBloom and lecturing internationally. He enjoys teaching and serves on advisory boards for local Vet Tech colleges, is on the Aratana Technician Council of Pain Experts and on multiple speaker bureaus. Stephen serves as the Past President for the Society of Laboratory Animal Veterinary Technicians, Vice President for the California RVT Association and member at large for the National Association of Veterinary Technicians in America. |