Tooth resorption in dogs and cats
Bonnie Shope, VMD, DAVDC and Diane Carle, DVM, DAVDC
Veterinary Dental Services, Boxborough, MA
Posted on 2017-02-07 in Dentistry
Tooth resorption is the progressive destruction of the calcified substance of permanent teeth by clastic cells.1 It can be extremely painful and is one of the most common oral diseases seen in cats.2,12,18 It is also frequently found in dogs. Despite the high prevalence of this disease, there is confusion about nomenclature, classification, diagnosis and treatment in the veterinary profession, and much remains unknown in both veterinary dentistry and human dentistry about this condition. The current state of understanding of this important oral disease is reviewed here, including the accepted nomenclature and classification of types of tooth resorption, methods for diagnosing tooth resorption, the etiology of the disease, and recommendations for treatment in dogs and cats.
Nomenclature and classification of tooth resorption
The nomenclature of tooth resorption has evolved over time and multiple names are used in veterinary literature, particularly in reference to feline tooth resorption. The currently accepted term is “tooth resorption,” which is divided into subcategories using several different classification schemes that are described below. Tooth resorption has been called cat caries, or cat cavities, but this is incorrect because caries is the result of destruction of mineralized tissues from acid produced by bacteria, whereas in fact, clastic cells carry out tooth resorption. They have been called neck lesions or cervical line lesions, but this is inappropriate because the lesions are found anywhere on the tooth. The term feline odontoclastic resorptive lesions (FORLs) is still sometimes used, but this is misleading because the process of resorption in feline teeth appears to be identical to that in teeth of other species and the use of the synonyms odontoclastic and resorptive is redundant.
Tooth resorption in dogs and cats is currently classified using several different schemes. The American Veterinary Dental College (AVDC) originally used a classification scheme based on the extent of the resorptive lesion, but has recently incorporated an additional classification based on the radiographic appearance of the lesions.
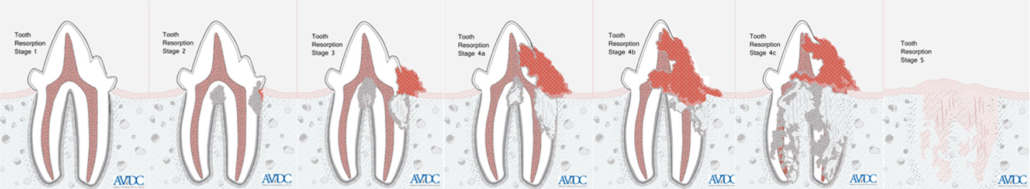
The original AVDC scheme (fig. 1) is:
- Stage 1 (TR1): Mild dental hard tissue loss (cementum or cementum and enamel)
- Stage 2 (TR2): Moderate dental hard tissue loss (cementum or cementum and enamel with loss of dentin that does not extend to the pulp cavity).
- Stage 3 (TR3): Deep dental hard tissue loss (cementum or cementum and enamel with loss of dentin that extends to the pulp cavity); most of the tooth retains its integrity.
- Stage 4 (TR4): Extensive dental hard tissue loss (cementum or cementum and enamel with loss of dentin that extends to the pulp cavity); most of the tooth has lost its integrity.
- TR4a: Crown and root are equally affected.
- TR4b: Crown is more severely affected than the root.
- TR4c: Root is more severely affected than the crown.
- Stage 5 (TR5): Remnants of dental hard tissue are visible only as irregular radiopacities and gingival covering is complete.
Some authors found this scheme limiting because it did not describe the location (other than root or crown) or radiographic pattern of the lesions, and it did not address the cause of the resorption.3
Dupont and DeBowes divided resorptive lesions into two types: Type 1, characterized by roots with normal appearance of the periodontal ligament space, and radiodensity similar to adjacent tooth roots, and Type 2, with extensive root replacement by alveolar bone and roots that are radiolucent when compared to adjacent tooth roots. This classification provides clinically useful information regarding treatment, with teeth with Type 1 resorption requiring complete extraction and teeth with Type 2 resorption being suitable candidates for crown amputation with intentional root retention.38 The AVDC incorporated this classification into its scheme and added a third type, Type 3, where characteristics of both Type 1 and Type 2 resorption are present on the roots of a single tooth.
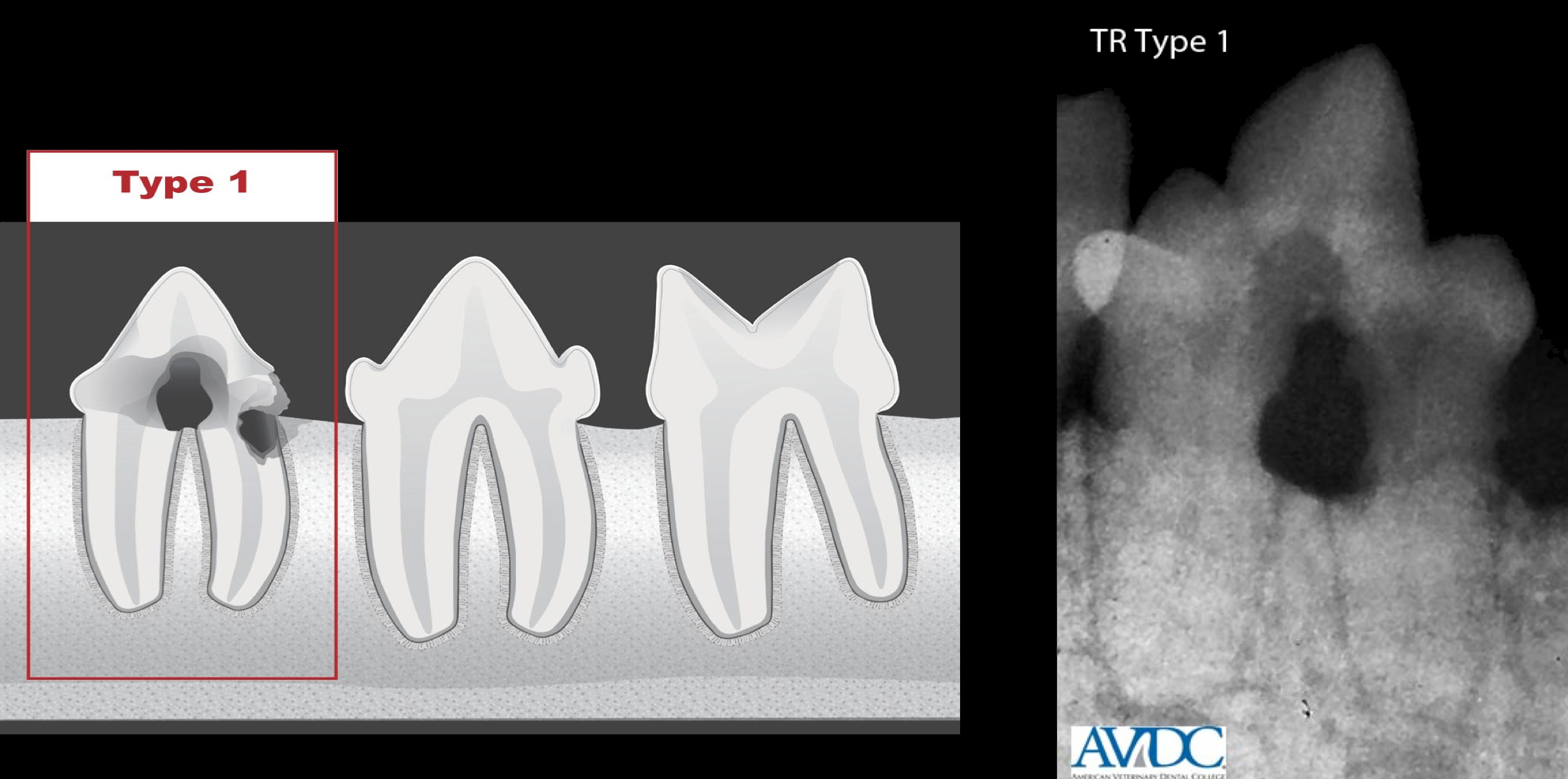
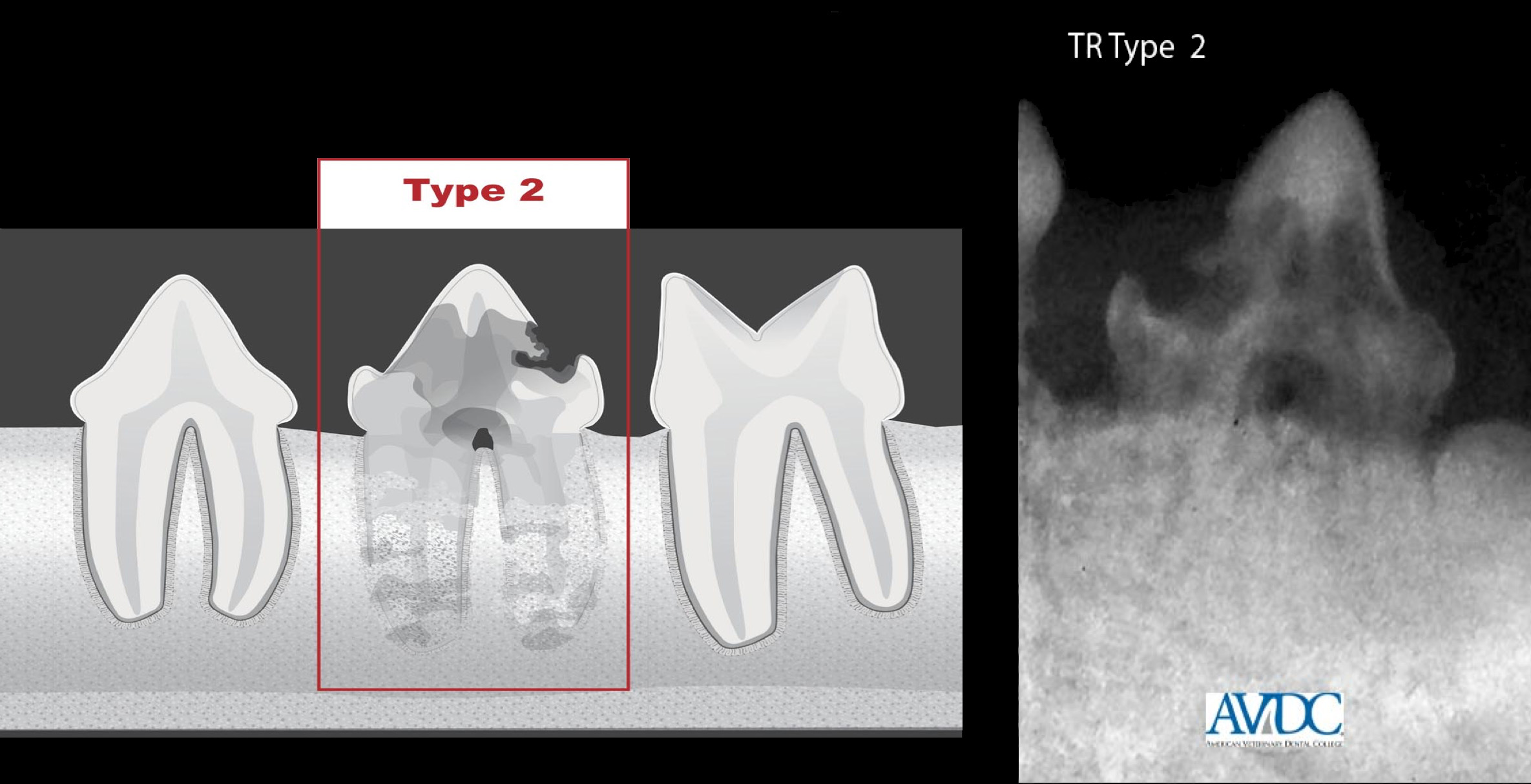
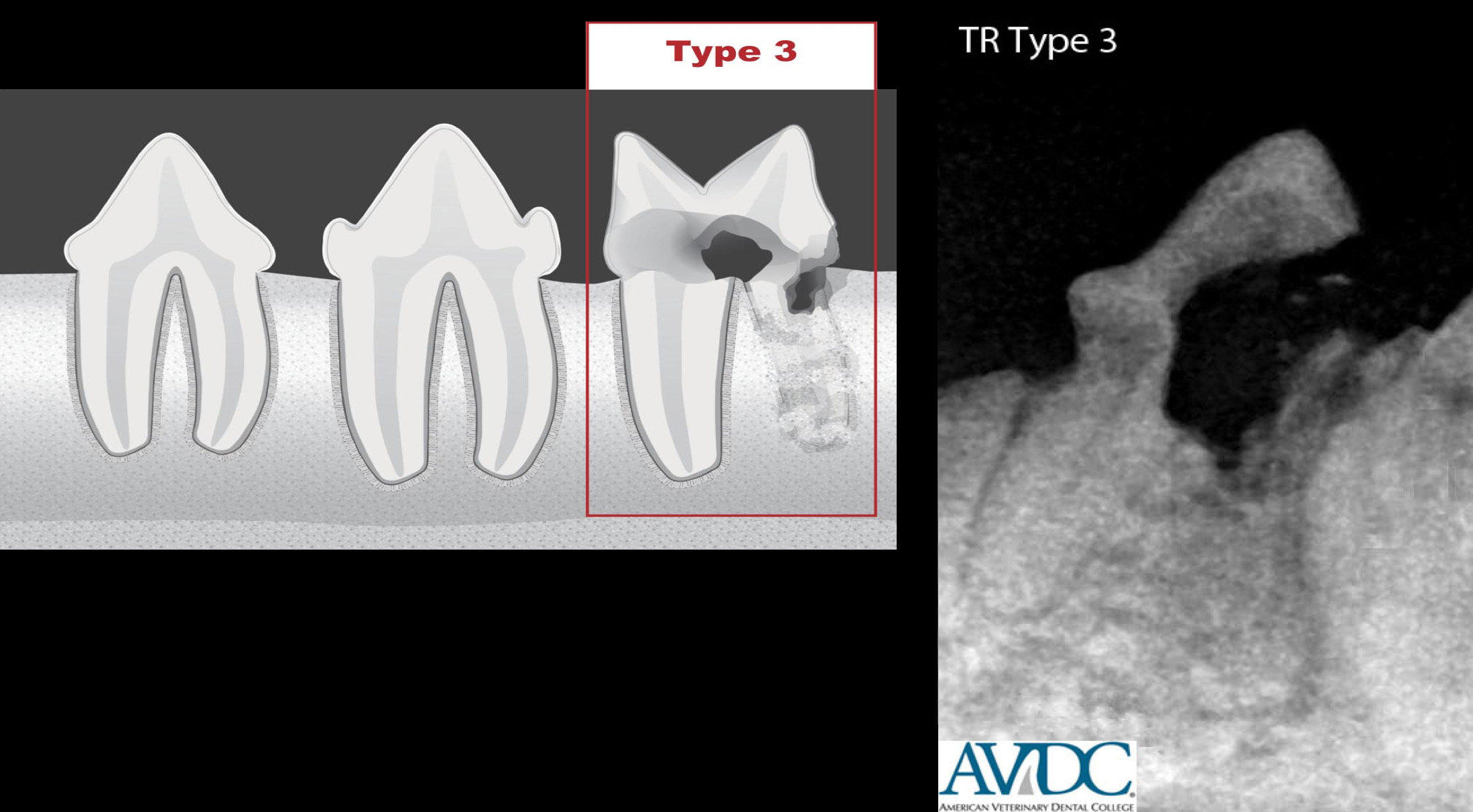
The current classification (fig. 2) based on radiographic appearance is:
- Type 1: On a radiograph of a tooth with type 1 (T1) appearance, a focal or multifocal radiolucency is present in the tooth with otherwise normal radiopacity and normal periodontal ligament space.
- Type 2: On a radiograph of a tooth with type 2 (T2) appearance, there is narrowing or disappearance of the periodontal ligament space in at least some areas and decreased radiopacity of part of the tooth.
- Type 3: On a radiograph of a tooth with type 3 (T3) appearance, features of both type 1 and type 2 are present in the same tooth. A tooth with this appearance has areas of normal and narrow or lost periodontal ligament space, and there is focal or multifocal radiolucency in the tooth and decreased radiopacity in other areas of the tooth.6
These classification schemes are intended to be combined so that a tooth with a Stage 4b lesion that has a type 2 radiographic appearance would be abbreviated TR-S4b-T2.6
Fig. 2: Stage of tooth resorption (click to advance through slides). First 3 images used with permission © AVDC®
Other authors have investigated the suitability of using a widely accepted human resorption classification scheme8 to classify tooth resorption in dogs.3 The human scheme uses 7 types of resorption based on radiographic appearance: 1) external surface resorption, 2) external replacement resorption, 3) external inflammatory resorption, 4) external cervical root surface resorption, 5) internal surface resorption, 6) internal replacement resorption and 7) internal inflammatory resorption.
In this study, the two most common types of tooth resorption found in dogs were external replacement and external inflammatory resorption. External cervical root surface resorption, external surface resorption, internal inflammatory and internal surface resorption were uncommon in this study, and internal replacement resorption was not found.3
Table 1 describes the types of tooth resorption described in the study based on the human classification scheme. These terms are frequently used in both veterinary and human literature.
Prevalence of tooth resorption in dogs and cats
The prevalence of tooth resorption has been extensively studied in cats but there are only a few studies of the prevalence of tooth resorption in dogs. In domestic cats tooth resorption is reported to be one of the most common oral conditions, although the reported prevalence varies widely because there is substantial variation in methods used to diagnose tooth resorption (oral exam only versus exam and radiographs) as well as the population studied (healthy animals, animals presenting to general practice, animals presenting to dental specialty practice). Reported prevalence of tooth resorption in cats ranges from 20 – 72%.2 The prevalence, as well as the number of teeth affected per cat increases with age.2,9,10 In one study the risk of a cat developing tooth resorption was found to increase 1.78 times with every year a cat aged.2 The youngest cat reported with tooth resorption was 1 year old.
There is some evidence that the prevalence in domestic cats has increased since the 1960’s leading some researchers to speculate that factors related to changes in feeding or care have influenced the prevalence.
In cats, two studies found that the mandibular third premolar tooth was the most commonly affected by tooth resorption2,9 while another study found that the fourth maxillary premolar and fourth mandibular premolar were the most commonly affected teeth.12 Lesions are often bilateral in cats.2
A study in the Netherlands21 found that Asian shorthaired cats, primarily Siamese cats were the most common cat breeds to be affected by tooth resorption, while a study in the United States found no difference in prevalence by breed.12
Prevalence in dogs has been reported to be 17.9% of randomly selected dogs in one study, and 21.7% of dogs in another study. Another study found that 53.6% of dogs presenting to a dental specialty practice had radiographic evidence of tooth resorption3 but few other, if any, studies of prevalence of tooth resorption have been conducted in dogs. In the study performed at the dental specialty practice, castrated males had a higher prevalence of tooth resorption than females or intact males, and there was a positive correlation with age. With the most common type of tooth resorption in dogs, external replacement resorption, there was a positive correlation with body weight and age and no association with concurrent dental disease.3
Signs and diagnosis of tooth resorption
Tooth resorption has been reported to cause anorexia, ptyalism, lethargy, depression, halitosis and discomfort. In the experience of the authors, tooth resorption rarely causes behavior changes in pets that are observable by owners, even when lesions are present that elicit signs of pain when probed under anesthesia. However, owners often notice increased energy and activity when teeth with painful resorptive lesions are removed.
Diagnosis of resorptive lesions begins with an awake oral examination. Crowns of teeth with resorptive lesions often have anywhere from a “pink spot” of tissue to extensive soft tissue visible on the crown, where gingival tissue and granulation tissue has grown into the lesion. Tooth extrusion or supereruption (movement of tooth beyond normal occlusal plane) is often associated with aging and periodontal disease, but is also a symptom of tooth resorption in cats.
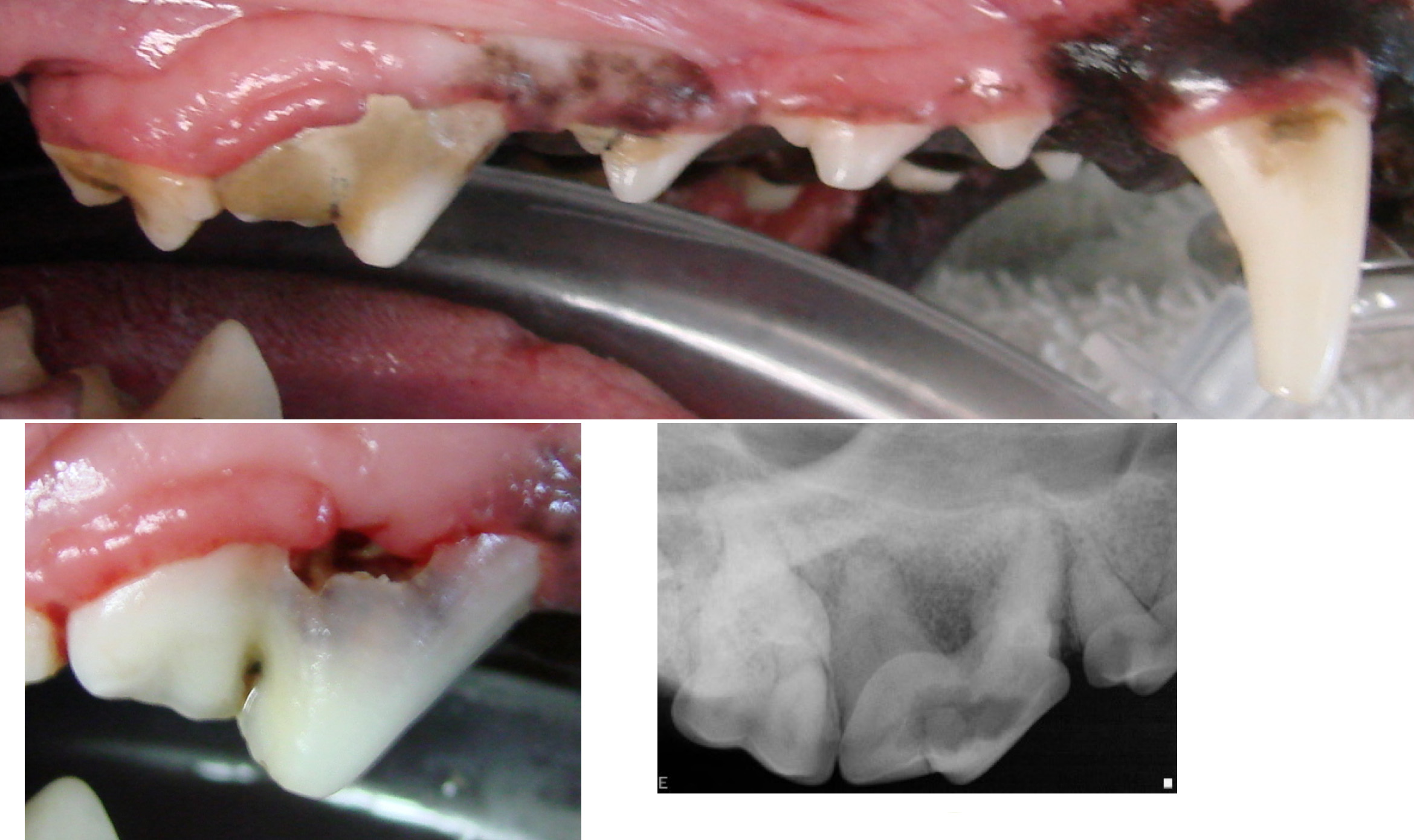
Fig. 3: It is easy to miss resorptive lesions on the awake exam because there is often calculus often covering lesions. Once the calculus is removed, the lesion becomes more readily apparent.
Smaller lesions are sometimes difficult to distinguish from areas of gingival enlargement during an awake oral examination, but are readily distinguishable during oral exam under anesthesia by the presence of a defect in the tooth. Often the crowns of teeth are obscured by calculus so it is not possible to visualize resorptive lesions until the teeth are scaled under anesthesia (fig. 3). There is a high correlation between number of missing teeth in the cat and the presence of tooth resorption,9 and missing teeth should increase suspicion for tooth resorption in cats. One study found no correlation between number of teeth and tooth resorption in dogs suggesting that tooth resorption in dogs might not progress to spontaneous fracture as readily as in cats.3
Furcation exposure (exposure of the division between the roots) from periodontal disease and subsequent bone loss can sometimes be confused with coronal resorptive lesions. Resorptive lesions frequently occur near the furcation, however, when resorptive lesions are probed during oral examination under anesthesia, they typically have a sharp enamel edge and an audible “tink” can be heard as the probe catches on the edge of the lesion. In contrast, furcation exposure tends to have a smooth gradual edge when probed. While probing resorptive lesions during the awake exam or under anesthesia often elicits a pain response such as chattering, this is not pathognomonic for tooth resorption. Some cats also exhibit chattering under anesthesia if inflamed gingiva from periodontal disease or stomatitis is probed.
Resorption is sometimes mistaken for carious lesions in dogs. (Caries should not be a differential for tooth lesions in the cat, as only one report of caries in cats can be found in the literature from skulls found in a 13th century excavation). Resorption in dogs can be distinguished by the location of the lesion and the characteristics of the lesion based on probing. Caries tends to occur on occlusal surfaces, while resorption tends to extend onto non-occlusal surfaces. Carious lesions have abnormally soft enamel and/or dentin while resorptive lesions usually have hard dentin.
Regardless of the findings on awake oral examination, it is beneficial to prepare owners for the likelihood that resorptive lesions may be discovered after a dental cleaning, oral examination under anesthesia and full mouth radiographs, especially in older cats, given the high prevalence of this disease in these patients.
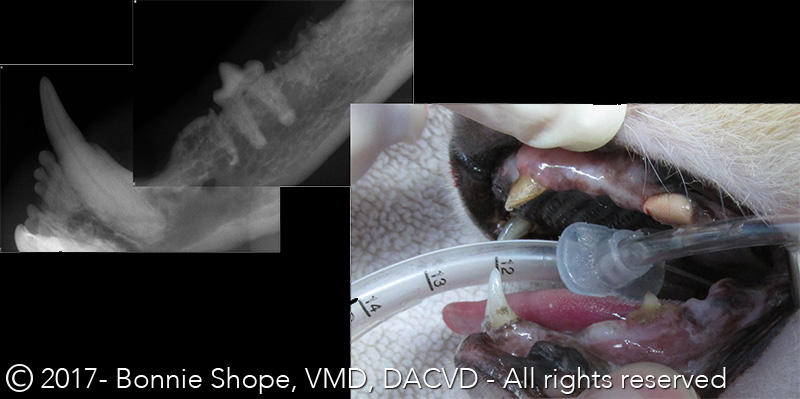
Fig. 4: Missing teeth are highly correlated with tooth resorption in cats, but not so in dogs. Dental radiographs are always recommended for both cats and dogs.
Radiographs are essential in diagnosing tooth resorption (fig. 4). A study of tooth resorption in the mandible of cat cadavers found 2.4 times as many teeth with tooth resorption after radiographs than with clinical examination alone and a study of feline patients in a dental specialty practice found an increase in diagnosed tooth prevalence from 53% of cats with oral examination only to 61% after radiographs.
Tooth resorption can appear radiographically in a variety of ways depending on the type of resorption present. This is outlined in detail in Table 1 above. In general, tooth resorption can appear as radiolucency in the crown or root, focal enlargement of the root canal, loss of periodontal ligament detail focally or throughout the root, or virtual disappearance of the root with only a faint remnant visible or complete.16 Overexposure of the cervical area of the tooth in cats can resemble tooth resorption so careful exposure of radiographs is important.
It is interesting that a histological study of clinically and radiographically unaffected teeth in cats with evident tooth resorption in other teeth found histological evidence of tooth resorption in 60% of the apparently normal teeth, indicating that early lesions are often present and difficult to diagnose in cats with a history of tooth resorption.
Etiology of tooth resorption
Despite the high prevalence of tooth resorption in dogs, cats and humans, surprisingly little is understood about the etiology. In particular, the cause of the extremely high prevalence in cats is not understood.
At the cellular level, some progress has been made in understanding tooth resorption. Resorption is carried out by odontoclasts. Odontoclasts appear to be similar and, most likely, identical to osteoclasts histologically, ontologically and biochemically. Both osteoclasts and osteoblasts derive from hematopoietic stem cells in the bone marrow or spleen. These cells follow the maturation pathway of macrophages until the final differentiation steps, where they develop into osteoclast precursors. The precursors migrate throughout the body and fuse together to become multinucleated mature clastic cells when stimulated. Odontoclasts are most likely osteoclasts that have migrated to and matured in vessels of alveolar bone or the periodontal ligament.22,24
A mature odontoclast attaches itself to the tooth surface by bonding to specific proteins in calcified tissue in bone or teeth. The ruffled cell membrane that distinguishes osteoclasts from other cells contacts the tooth surface. The attachment forms a sealed resorption compartment, which restricts the clastic activity to area of the tooth contained within the seal. Intracellular vesicles containing hydrogen ions and proteolytic enzymes fuse with the ruffled odontoclast membrane, releasing their contents and dissolving the hard tissue of the tooth to which they are attached.1
Odontoclasts can attach anywhere on the root surface or at several locations simultaneously but appear to only rarely attach to enamel surfaces. Resorption then progresses from the cementum coronally into the crown dentin and apically into the root dentin.13
The mystery of tooth resorption is why adult teeth become vulnerable to destruction by mineralized tissues. Healthy adult teeth are protected from these clastic cells by the resorption-inhibiting characteristics of unmineralized layers on external and internal root surfaces. These structures include the periodontal ligament, cementoblasts, cementum, odontoblasts and predentin (the collagen matrix created by cementoblasts before maturation and mineralization).1,13
Even if these inhibitory mechanisms fail, in adult human teeth, external resorption is limited by simultaneous repair.13 Histologic studies of resorption in feline teeth show that resorption and repair are occurring simultaneously., However, in feline teeth, resorption outpaces repair until the root is completely resorbed and the crown breaks off.2
In human dentistry, the prevailing theory of tooth resorption is that damage to the normal protective barriers to resorption, combined with inflammation adjacent to the root surface, initiate resorption and persistent stimulation results in a clinical resorptive lesion.1 This may occur in humans with pulpal disease, periodontal disease, trauma, exposure to high temperatures, chemical damage such as bleaching, viruses (although evidence for this is extremely weak), and pressure secondary to orthodontic movement, tooth impaction or expansive pathological lesions.1 Oral bacteria in humans have also been shown to stimulate osteoclast differentiation.1 There are also reports in the human literature of idiopathic tooth resorption that may be related to genetic alterations in interleukin 1.1
Research in humans regarding tooth resorption can provide useful data for understanding resorption in dogs and cats, but must be interpreted with caution as there are some substantive differences in the prevalence and progression of tooth resorption in humans compared with dogs and cats. For example, in humans, external surface resorption is considered reversible and infrequent. In dogs this condition is also infrequent but it is often associated with external replacement resorption suggesting that disease progresses to external replacement resorption.3 Furthermore, external replacement resorption is common in dogs3 and cats,27 but rare in humans.3 It is idiopathic and not associated with clinical signs in dogs and does not require treatment. In contrast, in humans, this type of resorption is progressive and usually associated with necrosis of the periodontal ligament, intrusive injuries, or delayed replantation of avulsed teeth.3
Multiple theories as to why feline teeth are vulnerable to resorption have been proposed but none, to date, have been confirmed. Inflammation from periodontal disease has been suggested as a cause for tooth resorption in cats. Inflammation of periodontal tissue and subsequent release of cytokines and lipopolysaccharides has been shown to stimulate differentiation and migration of clastic cells.13 However, some studies have indicated that early external resorptive lesions do not appear to be associated with inflammatory cells, and it is possible that inflammatory cells are the result of, rather than the cause of, tooth resorption.13 Some studies have found no association between the presence of resorptive lesions and gingivitis,2, while others found that gingivitis was positively associated with tooth resorption.9,11 A study of periodontitis in cats and Type 1 vs. Type 2 found periodontitis was more than 8 times more likely to be present in teeth with Type 1 roots, but not more common in teeth with Type 2 resorption. One study of cats found the most significant risk factor for tooth resorption in cats was a history of dental disease.
Other factors implicated in the pathogenesis of feline tooth resorption include FIV , systemic acidosis, calcium regulation, local hypoxia, occlusal trauma from hard kibble, excess vitamin D in diets, 13overexpression of vitamin D receptors, or drinking city (vs. well) water. Cats from urban environments and indoor cats have been found to have a greater incidence of tooth resorption.29 In contrast, other studies found no association between tooth resorption and FIV (or FeLV),30 type of food fed,29 or water source.29
Histologic observations of teeth in animals affected by tooth resorption can shed some light on the etiology. Cats with tooth resorption often show excess deposition of cementum, called hypercementosis. Supereruption, or abnormal extrusion of teeth, particularly canine teeth, occurs commonly in cats with resorption lesions on other teeth. This may be the result of hypercementosis, or increased osteoblastic activity of periapical bone. Cats with tooth resorption also have been shown to have anatomical differences in the periodontal ligament including vascular and edematous morphology if ankylosis is present, or a narrower ligament lacking normal oblique and horizontal fiber bundles in the absence of ankylosis.21
Microhardness of feline tooth enamel and dentin is lower than in canine and human teeth.24 Feline teeth have vasodentin-like structures, or vascular dentin, that is typically found only in fish teeth. They also have been found to have areas of tooth structure resembling osteodentin, a rapidly formed dentin typically found in human teeth following trauma or with a condition called osteogenesis imperfecta. Osteodentin is also found normally in fish, and normal teeth in other mammals. The significance of these histological findings with respect to the high prevalence of tooth resorption in cats is not yet known.24
Treatment of tooth resorption
In the past, treatment for resorptive lesions in cats has included fluoride treatment for early lesions, and restoration or restoration with root canal for advanced lesions. However, studies of cats with tooth resorption treated with restoration with glass ionomer found that 72% showed progression of tooth resorption.18 Furthermore, while fluoride is effective in making teeth resistant to acid demineralization, such as that occurring with caries, it has not shown any efficacy in treating tooth resorption.18
Currently, treatment of tooth resorption is directed towards relieving the discomfort from tooth resorption and is limited to extraction (figs. 5 and 6) or crown amputation (fig. 7). Teeth with external replacement resorption where the lesion does not extend into the crown of the tooth are not believed to be painful and do not require treatment.26 In feline teeth with extensive root resorption, the crowns are at risk for spontaneous fracture due to extensive undermining, so crown amputation may be advisable for these teeth, even if resorption does not extend into the crown.
A study of dogs with resorption did not find significantly fewer teeth than those without resorption, so it appears that tooth loss caused by resorption is uncommon in dogs.3 This supports the suggestion that teeth with resorption, but no coronal involvement in dogs, most likely do not require any treatment.
Early resorptive lesions do not appear to be symptomatic. However, resorption is progressive, and these lesions have a high likelihood of progressing to a stage where they become painful. The rate of progression of resorptive lesions is unknown and appears to be widely variable. Pets belonging to clients who are willing to return for regular rechecks, including radiographs, may not require treatment of early lesions, but if return visits are unlikely it is advisable to extract teeth with early lesions to avoid painful advanced lesions in the future.
Some teeth are candidates for removal of the crown only, a procedure called crown amputation with intentional root retention. One study found that feline teeth with Type 2 tooth resorption treated with crown amputation and intentional root retention showed continued root resorption and replacement with bone for up to three years after treatment and that the teeth healed well with no future inflammation. A subsequent study also followed teeth in cats with Type 2 resorption treated with crown amputation and confirmed these results. Cats were examined at intervals ranging from 6 to 72 months and researchers found continued resorption, or no additional resorption but no signs of inflammation, in 96.4% of treated teeth. 3.4% of teeth had no further resorption and radiographic signs of inflammation, but these teeth appeared to have had Type 3 (mixed type 1 and 2) resorption and probably should have been treated with extraction. A radiographic study of teeth in cats found no association between periapical lucencies, indicative of endodontic disease, and tooth resorption, even in lesions that extended into the pulp, supporting crown amputation as a suitable treatment for teeth with Type 2 resorptive lesions.
Misinterpretation of these studies can lead to the incorrect assumption that crown amputation is appropriate treatment for any tooth with tooth resorption. Resorbing teeth are often challenging extractions and it is tempting to resort to crown amputation rather than extracting teeth. The only teeth suitable for crown amputation are those undergoing external replacement resorption of the roots with no visible periodontal ligament (Type 2 resorption). Teeth with Type 3 resorption must be fully extracted to avoid future infection and pain. Retained tooth roots resulting from the crown of teeth with Type 1 resorption breaking off must also be extracted. Furthermore, teeth with tooth resorption and any radiographic or clinical signs of periodontal or endodontic pathology must be extracted.38

Fig. 5: Treatment for tooth resorption depends on the type of lesion. Type 1 lesions must be extracted. These extractions can be challenging sometimes due to the weakness of the crown and the presence of some ankyloses even in Type 1 lesions. Removing buccal bone can help make the extractions easier.
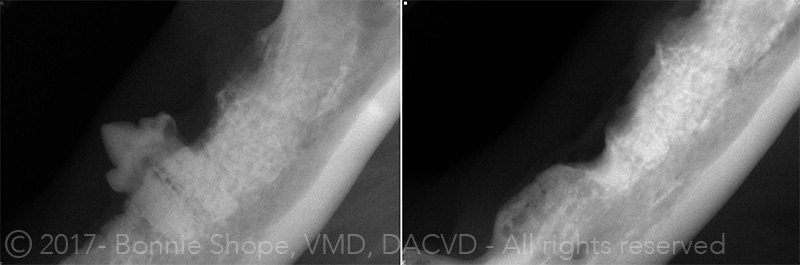
Fig. 7: Type 2 lesions can be treated with crown amputation with intentional root retention. Crown amputation is NOT appropriate for any teeth with tooth resorption except for those with type 2 radiographic appearance. This technique has been investigated in several studies and it was found that in teeth with Type 2 radiographic appearance the roots continue to resorb until they are completely replaced by bone. This is not suitable for Type 3 lesions.
Cats with stomatitis and dogs with chronic ulcerative paradental stomatitis (CUPS) frequently have concurrent tooth resorption in one or more teeth. When performing full mouth or cheek teeth extractions on these animals to treat stomatitis, it is essential that all tooth material is removed from the mouth, including resorbing roots.38 This is difficult and may involve substantial removal of alveolar bone to accomplish. These extractions may require referral to a veterinary dentist.
Little research has been performed regarding treatment for tooth resorption beyond extraction or crown amputation. A study in cats using Alendronate, a common bisphosphonate used in humans to treat osteoporosis, showed promising results for therapeutic use of the drug to treat tooth resorption in cats, but substantial additional research would be required before clinical use.22
A resorptive lesion in the mesial crown and mesialbuccal root of a maxillary fourth premolar tooth of a military working dog that was suspected to be internal inflammatory resorption caused by trauma was successfully treated by hemisection and extraction of the affected cusp of the tooth and both mesial roots and vital pulpotomy of the unaffected distal cusp of the tooth. The distal cusp and root appeared healthy at one year follow up.
Conclusion
Additional research is needed to elucidate the pathophysiology and etiology of tooth resorption in dogs and cats, and future investigations into treatments other than extraction or crown amputation will be important for this common but poorly understood dental disease.
References
- Darcey J, Qualtrough A. Resorption: part 1. Pathology, classification and aetiology. Brit Dent Jour 2013. 214(9):439-451.
- Ingham KE, Gorrel C. Prevalence of odontoclastic resorptive lesions in a population of clinically healthy cats. J Small Anim Pract 2001 42:439-443.
- Peralta S, Verstraete FJM, Kass PH. Radiographic evaluation of the types of tooth resorption in dogs. AJVR 2010; 71:784-793.
- Harvey CE, Orsini P, et al. Mapping the radiographic central point of feline dental resorptive lesions. J Vet Dent 2004;21:15-21.
- Dupont GA. Radiographic evaluation and treatment of feline dental resorptive lesions. Vet Clin Small Anim . 2005. Vet Clin Small Anim 35:943-962.
- www.avdc.org/nomenclature.html#resorption. Accessed 1/11/15.
- DuPont G,A DeBowes LJ. Comparison of periodontitis and root replacement in cat teeth with resorptive lesions. J Vet Dent 2002. 19(2):71-75.
- Andreasen FM, Andreasen JO. Luxation injuries of permanent teeth. General findings. In: Anreasen JO, Andreasen FM, Andersson L, eds. Textbook and color atlas of traumatic injuries to the teeth, 4th ed. Copenhagen: Blackwell Munksgaard 2007;372-403.
- Mestrinho LA, Runhau J, et al. Risk Assessment of feline tooth resorption: A Portuguese clinical case control study. J Vet Dent 2013 30(2):78-83.
- Coles S. The prevalence of buccal cervical root resorptions in Australian cats. J Vet Dent 1990 7(4):14-16.
- Harvey C, Shofer F. Epidemiology of periodontal disease in dogs and cats. Proceedings of the Annual Meetings of the American Veterinary Dental College 1992. 6 45-46.
- Van Wessum R, Harvey CE, Hennet P. Feline dental resorptive lesions. Prevalence patterns. Vet Clin N America. Small Animal Practice 1992 22(6):1405-1416.
- Reiter AM, Mendoza KA. Feline odontoclastic resorptive lesions. An unsolved enigma in veterinary dentistry. Vet Clin Small Anim 2002. 32:791-837.
- Hamp SE, Olsson SE, Farso-Madsen K. Radiography of spontaneous periodontitis in dogs. Vet Radiol Ultrasound 1984. Vet Radiol Ultrasound 25:86-92.
- Verstraete FJ, Kass PH, Terpak CH. Diagnostic value of full mouth radiography in dogs . AJVR 1998 59;686-691.
- Dupont GA. Radiographic evaluation and treatment of feline dental resorptive lesions. Vet Clin Small Anim . 2005. Vet Clin Small Anim 35:943-962.
- Berger M, Stich H, et. al. Feline caries in two cats from a 13th century architectural excavation. J Vet Dent 2006 23(1):13-7.
- Lyons KF. Subgingival odontoclastic resorptive lesions. Classification, treatment and results in 58 cats. Vet Clin N America. Small Animal Pract. 1992 22(6):1417-1432.
- Gengler W, Bubielzig R, Ramer J. Physical examination and radiographic analysis to detect dental and mandibular bone resorption in cats: a study of 81 cases from necropsy. J Vet Dent 1995, 12:97-100.
- Verstraete FJM, Kass PH, Terpa CH. Diagnostic value of full-mouth radiography in cats. AJVR 1998;59:692-695.
- Gorrel C, Larsson A. Feline odontoclastic resorptive lesions: unveiling the early lesion. J Small Anim Pract 2002 43:482-488.
- Mohn KL, Jacks TM et al. Alendronate binds to tooth root surfaces and inhibits progression of feline tooth resorption: a pilot proof of concept study. J Vet Dent 2009 26(2):74-81.
- Reiter AM. Biology of alveolar bone and tooth resorbing cells. Proceedings of the 12th Annual Veterinary Dental Forum. New Orleans, 1998. P 225-7.
- Okuda A, Harvey CE. Etiopathogenesis of feline dental resorptive lesions. Vet Clin North America Small Animal Practice 1992 22(6):1385-1404.
- Reichart PA, Durr Um, et. al. Periodontal disease in the domestic cat. A histopathological study. J Perio Res 1984;19:67-75.
- Arnjberg J. Idiopathic dental root resorption in old dogs. J Vet Dent 1996. 13(3):97-99.
- Ingham KE, Gorrel C, et. Al. Prevalence of odontoclastic resorptive lesions in a population of clinically healthy cats. J Small Anim Pract. 2001 42:439-443.
- DuPont GA, DeBowes LJ. Comparison of periodontitis and root replacement in cat teeth with resorptive lesions. J Vet Dent 2002, 19(2):71-75.
- Scarlett JM, Saidla J, Hess J. Risk factors for odontoclastic resorptive lesions in cats. JAAHA 1999;35:188-92.
- Hofmann-Lehmann R, Berger M, et. al. Feline immunodeficiency virus (FIV) infection lead to increased incidence of feline odontoclastic resorptive lesions (FORL). Vet Immunol Immunopathol 1998, 65;299-308.
- Muzylak M, Arnett TR, et. al. The in vitro effect of pH on osteoclasts and bone resorption in the cat: implications for the pathogenesis of FORL. J Cell PHysiol 2007 213:144-50.The in-vitro effect
- Reiter AM, Lyon KF, et al. Evaluation of calciotrophic hormones in cats with odontoclastic resorptive lesions. AJVR 2005, 66:1446-52.
- Muzylak M, Price JS, Horton MA. Hypoxia induces giant osteoclast formation and extensive bone resorption in the cat. Calcif Tissue Int 2006; 79:301-9.
- Burke FJT, Johnston N, Wiggs RB, Hall AF. An alternative hypothesis from veterinary science for pathogenesis of noncarious cervical lesions. Quint Int 2000; 31:475-482.
- Booij-Vrieling HE, Tryfonidou MA, et al. Inflammatory cytokines and the nuclear vitamin D receptor are implicated in the pathophysiology of dental resorptive lesions in cats. Vet Immun and Immunopath 2009 132:160-166.
- Lund EM, Bohacek LK, et al. Prevalence and risk factors for odontoclastic resorptive lesions in cats. JAVMA 1998 212(3):392-5.
- Lewis JR, Okuda A, et al. Significant association between tooth extrusion and tooth resorption in domestic cats. J Vet Dent 2008 25(2):86-95.
- Dupont G. Crown amputation with intentional root retention for advanced feline resorptive lesions: a clinical study. J Vet Dent 1995;12:9-13.
- Mihaljevic S-Y, Kernmaier A, Mertens-Jentsch S. Radiographic changes associated with tooth resorption Type 2 in cats. J Vet Dent 2011;29(1):20-26.
- Lommer MJ, Verstraete FJM. Prevalence of odontoclastic resorption lesions and periapical radiographic lucencies in cats: 265 cases (1995-1998). JAVMA 2000. 217(12):1866-1869.
- Eikenberg S, Loheide H, Arens FC. Treatment of asymptomatic internal resorption of a maxillary premolar tooth in a military working dog. 1998 J Vet Dent 15(4):175-178.
About the authors
Dr. Bonnie Shope
Dr. Shope is a diplomate of the American Veterinary Dental College. She graduated from the University of Pennsylvania School of Veterinary Medicine in 1997, and from Brown University with a Bachelor of Arts in 1991. As a veterinary student, Dr. Shope developed an interest in veterinary dentistry. She practiced small animal medicine after graduation, and then joined Veterinary Dental Services in 2000. From 2002 – 2007 she also worked as a Clinical Assistant Professor at the Cummings School of Veterinary Medicine at Tufts University.
Dr. Diane Carle
Dr. Carle is a diplomate of the American Veterinary Dental College. She graduated from Tufts University School of Veterinary Medicine and Swarthmore College, and worked in mixed practice before joining Veterinary Dental Services, LLC in 2010. She lives with her two cats, Kitten and Quinn, a rescue kitty who had surgery and two root canals at VDS to treat an unhealed jaw fracture. Quinn is fully recovered from his surgery.

Bonnie Shope, DVM, DAVDC

Diane Carle, DVM, DAVDC