Chronic kidney disease
Julie Fischer, DVM, DACVIM (SAIM)
Veterinary Specialty Hospital, San Diego, CA
Posted on 2019-07-26 in Internal Medicine
Physiology and pathophysiology
“CRF” or “CKD,” usually refers to progressive, irreversible, ongoing tubulointerstitial nephritis (which we’ll call CKD from here on out). In order to diagnose CKD, we must document:
- subnormal concentrating ability (cats <1.035, dogs<1.030)
- renal azotemia (traditionally with creatinine)
- persistence (>3-6 weeks)
Serum symmetric dimethylarginine (SDMA) is a relatively new blood marker used to detect and track decreasing renal function. Like creatinine it’s entirely renally excreted, but unlike creatinine, it’s not affected by body mass. In an animal with incipient CKD, SDMA may increase a year or more before creatinine does, thus monitoring of SDMA may aid earlier CKD detection.
Once CKD is confirmed, it’s helpful to classify it by stage/substage. IRIS (the International Renal Interest Society) bases staging of CKD on creatinine measurement, then designates substages by the presence or absence of hypertension and proteinuria. We know that the presence of either condition will speed renal deterioration, and that controlling either or both when present will slow disease progression, thus these characteristics have prognostic implications. Using the IRIS grading system gives us consistency and a common language for discussing clinical signs, therapies, and prognoses along a continuum of disease progression. Here’s the IRIS website with staging guidelines and reference cards: http://iris-kidney.com/guidelines/staging.html
The presence of CKD can cause derangement in all renal functions, including:
- body water and electrolyte balance
- solute excretion and reclamation by passive diffusion and active reabsorption and secretion in the renal tubules
- acid/base modulation by HCO 3 reabsorption, NH 3 production, and H + excretion
- synthesis of many different hormones and cytokines (erythropoietin, calcitriol, prostaglandins, kinins, renin)
*For IRIS stage 1-2 disease: focus on diet change and hypertension/proteinuria management to slow progression.
*For IRIS stage 3-4 disease: target the inevitable clinical consequences of CKD.
Therapies for CKD
Nutrition
In stage 1-2 CKD, we rely on diet modification, used for CKD in pets for >50 years. “Renal diets” have protein reduced to maintenance level (not below, as many owners believe), reduced phosphorus/phosphate (P) and sodium; increased soluble fiber; and increased B-vitamins, buffers, potassium, omega-3 fatty acids, and antioxidants. Use of a renal diet in cats/dogs is the only therapy with Grade 1 evidence showing increased time until uremic crisis occurs, and decreased mortality. There is no single modification that this results from; rather it results from the sum of the modifications
- Potassium supplementation: Most dogs with CKD who are still eating don’t get hypokalemic, but cats do and K + depletion may decrease glomerular filtration rate (GFR) which is a measure of renal function. Severely hypokalemic cats (K < 2.5 mmol/L) have muscular weakness and may have cervical ventroflexion. For most cats, supplementation beyond that already present in most commercial renal diets is not needed. For some, potassium gluconate is helpful.
- Increased omega-3 polyunsaturated fatty acids (n-3 PUFA): Dogs with CKD fed n-3 PUFA supplemented diets have decreased mortality, fewer histopathological renal lesions, decreased proteinuria, and lower cholesterol levels than dogs fed diets high in saturated fats and n-6 fatty acids.
- Protein moderation: Limiting protein intake decreases uremia in stage 2-4 dogs/cats, likely because protein metabolism creates nitrogenous uremic toxins as well as additional acids. Whether to restrict protein in stage 1-early 2 nonproteinuric CKD patients is unclear, but better dietary acceptance and possible delay in onset of uremia favor using renal diets in the earliest stages of CKD. Maintenance-level protein restriction is benign in early-stage CKD, and is documented to be beneficial in stage 2 cats, therefore it is recommended when creatinine > 2.0 mg/dL.
Antiemetics/gastroprotectants
Most uremic signs are localized to the GI tract: anorexia, vomiting, stomatitis, glossitis, uremic gastropathy, mucosal ulceration, melena, diarrhea, tongue margin/tip necrosis, among others. Therapy for nausea/decreased appetite is usually needed by late stage 3. Vomiting occurs by direct stimulation of the chemoreceptor trigger zone in the brain, as well as from direct stimulation of the stomach and duodenum by uremic gastritis or gastropathy (chiefly in dogs). Anorexia may be nausea-associated, and/or can arise from uremic gastropathy, as well as from lack of excretion of appetite-suppressing toxins (like leptin).
Uremic stomatitis/glossitis occurs in later stages or with acute severe uremia, and results in fibrinoid necrosis and arteritis, chiefly on ventrolateral tongue margins/buccal mucosa (cats), and buccal mucosa/rostral tongue margins (dog). Degradation of salivary urea into ammonia contributes to stomatitis/glossitis, and to fishy uremic halitosis. Antiemetics (e.g., maropitant, ondansetron, metoclopramide [for dogs]), topical/systemic analgesics and antibacterials for oral ulceration, +/- H 2 blockers, and sucralfate if ulcers or erosions are present or suspected palliate signs, but changing the changeable (hypovolemia, infection, hypertension, proteinuria, systemic illness) and supporting return to a non/less uremic state are the ultimate keys.
Appetite stimulants
Appetite stimulants (mirtazapine especially, which decreases vomiting in cats as well) work variably well depending on severity of signs. If insufficient intake of prescribed diet persists (inability to maintain BCS 4), enabled feeding with an esophageal (or, less commonly, PEG) tube is an excellent option, and there really are no alternatives for persistent hyporexia, short of transplantation or dialysis. Early institution of enabled feedings (when the pet can’t maintain BCS of BCS ≥ 4 eating a renal diet) with a feeding tube can make a huge difference in quantity and quality of life.
Management of hypertension
Up-regulation of the renin-angiotensin-aldosterone system (RAAS), sympathetic nervous system stimulation, and other factors can lead to systemic hypertension, thus frequent BP measurement on calm patients is critical. When measuring BP, note cuff size, equipment type, extremity used, mental state (the patient’s!), and current medications at each assessment. We don’t treat a single elevated BP measurement, unless damage to end-organs (eye, brain, kidney, heart) is present (retinal hemorrhages or detachments, hyphema, stroke, seizure, dullness, concentric left-ventricular hypertrophy). My first-line drug for hypertension is amlodipine, a calcium channel blocker (CCB) that decreases BP by systemic arterial dilation. CCBs preferentially dilate afferent renal arterioles (that carry blood into the glomerular capillaries), so if BP stays uncontrolled, the glomeruli become vulnerable to hydraulic damage. Because of this, documentation of BP control is a must when using CCBs, and some clinicians simultaneously start an ACEi (which preferentially dilates efferent arterioles that carry blood our of the glomerular capillaries) to help prevent pressure damage. Usually aggressive and conscientious use of amlodipine suffices in hypertensive, non-proteinuric pets.
Alkalinization
Acidosis stems from decreased reabsorption and regeneration of HCO3- in the proximal tubule, decreased ability of the distal tubule to excrete hydrogen ions, and decreased GFR. Biochemical evidence of acidosis appears in later-stage CKD, but decreased buffering capacity starts early, and can be managed with supplemented buffer. Acidosis causes nausea, anorexia, vomiting, lethargy, weakness, and malaise. It causes protein catabolism and decreased ability to deal with other acid stress (diarrhea, dehydration, respiratory acidosis), increases bone demineralization, and can impair cardiac function and increase vasoconstriction. Most renal diets add potassium citrate as a buffer, and sodium bicarbonate is also a cheap, effective buffer if needed. Though buffering makes physiologic sense, we lack evidence to justify recommending it routinely, so it should be considered on a case-by-case, risk/benefit basis.
Control of phosphorus (P)
Phosphorus is a uremic toxin, and P retention leads to renal secondary hyperparathyroidism (hyperPTH), soft tissue (including renal) mineralization, reduced calcitriol levels, and enhanced disease progression. We target P = 2.7-4.5 mg/dL, sometimes not feasible in stage 4 disease, and decrease blood levels by limiting intake and decreasing gut absorption. Oral phosphate binders limit GI P absorption and complex with P in intestinal ingesta, preventing absorption. Aluminum, calcium, sevalamer, and lanthanum based binders are used in dogs/cats, and are most effective when used with P-restricted diets. P leaches from tissues and takes several weeks to equilibrate. Calcitriol has been extensively used in CKD dogs and cats, and normalizes PTH. We have strong (grade I) evidence in dogs with stage 3-4 CKD for low-dose calcitriol use to decrease mortality and slow disease progression. We lack strong evidence in cats.
Minimization of proteinuria
Proteinuria can both cause and worsen tubulointerstitial damage, so screening for and quantifying renal proteinuria and minimizing it with diet and ACEi are critical. If proteinuria is persistent and significant, a specific diagnostic investigation into possible causes is warranted.
Anemia management
Anemia usually develops in stage 3-4 disease, and frequently causes lethargy, decreased appetite, and increased respiratory/heart rates. Anemia may promote disease progression via hypoxic/ischemic renal injury and increased oxidative stress. Development is chiefly due to decreased renal cortical production of erythropoietin (EPO), but other causes include:
- GI blood loss from gastritis
- platelet dysfunction from uremic toxins
- decreased RBC lifespan from cell wall changes
- increased blood sampling for testing
EPO is a hormone made by fibroblasts living in the renal cortex, which detect changes in blood oxygen concentration and control hematocrit by increasing or decreasing EPO production accordingly. Normal marrow produces more RBC progenitors than needed, so extra progenitors undergo apoptosis (programmed cell death). When blood oxygen decreases, EPO is an antiapoptotic hotline for progenitors, signaling them to mature into RBCs. Renal cortical damage/fibrosis damages EPO-producing fibroblasts, EPO declines, and nonregenerative anemia develops. Erythropoietic hormone replacement can quickly improve this type of anemia. Recombinant human erythropoietin (Procrit, Epogen) was first used, but has now been supplanted by darbepoetin (DPO; Aranesp) due to high rates of antibody formation with the Procrit/Epogen. DPO’s side-chain glycosylation and molecular folding pattern decrease antigenicity, and development of anti-DPO antibodies is rarely reported. Iron dextrans are given at the first dose of erythropoietic therapy, but rarely need to be repeated.
Therapeutic recommendations in a nutshell
- Stage 1-2: Nutrition, nutrition, hydration, nutrition!
- Stage 3-4 and beyond: Nutrition, nutrition, nutrition; control uremic signs; hydration; normotension; minimize proteinuria; treat anemia; nutrition!
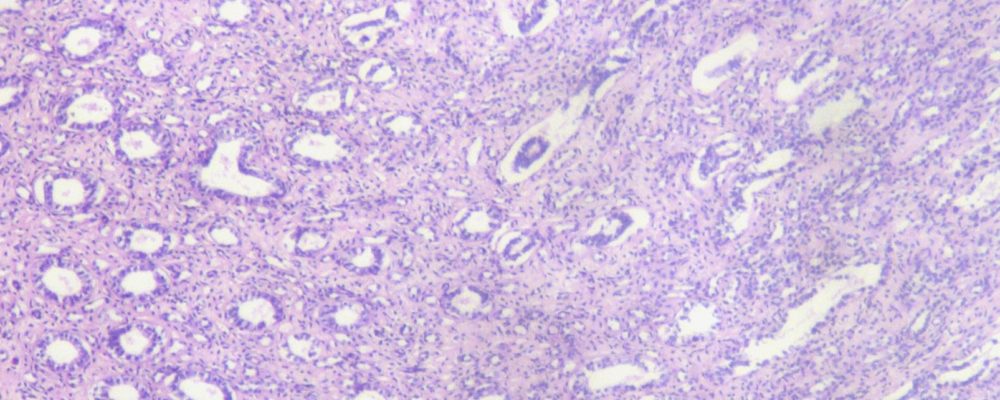
Image at top of page modified & used with permission by Jpogi at English Wikipedia [Public domain], via Wikimedia Commons” href=”https://commons.wikimedia.org/wiki/File:Kidney-medulla.JPG.
About the author
|

 Dr. Fischer received her Doctor of Veterinary Medicine degree from the University of Tennessee, College of Veterinary Medicine. She completed an internship in small animal medicine and surgery at the Atlantic Veterinary College, University of Prince Edward Island, Canada, and a small animal internal medicine residency at Kansas State University. Dr. Fischer served as a clinical instructor at Kansas State before entering private specialty practice in San Jose, California. In 2002, Dr. Fischer established UC Davis’s Nephrology, Urology and Hemodialysis Service in San Diego, coordinating the program until 2009 and becoming a nationally recognized expert in upper and lower urinary tract disease. She has been a Diplomate of the American College of Veterinary Internal Medicine, specialty of Small Animal Internal Medicine, since 2000. Dr. Fischer particularly enjoys the diagnosis and management of upper and lower urinary tract problems, including complicated infections, obstructive ureteral diseases, prostatic diseases, incontinence, and acute and chronic renal failure. Her other special interests include immune-mediated diseases, oncology, and the clinical training of veterinary students and house officers. She served on the ACVIM Small Animal Internal Medicine Credentials Committee, and served on and chaired the Small Animal Internal Medicine Residency Training Committee. Dr. Fischer is passionate about the evolving art of post-doctoral veterinary education, especially the fusion of academic and private-practice advanced training programs. She has published scientific journal articles and textbook chapters on urinary diseases and other internal medicine topics, and speaks locally, nationally, and internationally on topics in nephrology and urology.
Dr. Fischer received her Doctor of Veterinary Medicine degree from the University of Tennessee, College of Veterinary Medicine. She completed an internship in small animal medicine and surgery at the Atlantic Veterinary College, University of Prince Edward Island, Canada, and a small animal internal medicine residency at Kansas State University. Dr. Fischer served as a clinical instructor at Kansas State before entering private specialty practice in San Jose, California. In 2002, Dr. Fischer established UC Davis’s Nephrology, Urology and Hemodialysis Service in San Diego, coordinating the program until 2009 and becoming a nationally recognized expert in upper and lower urinary tract disease. She has been a Diplomate of the American College of Veterinary Internal Medicine, specialty of Small Animal Internal Medicine, since 2000. Dr. Fischer particularly enjoys the diagnosis and management of upper and lower urinary tract problems, including complicated infections, obstructive ureteral diseases, prostatic diseases, incontinence, and acute and chronic renal failure. Her other special interests include immune-mediated diseases, oncology, and the clinical training of veterinary students and house officers. She served on the ACVIM Small Animal Internal Medicine Credentials Committee, and served on and chaired the Small Animal Internal Medicine Residency Training Committee. Dr. Fischer is passionate about the evolving art of post-doctoral veterinary education, especially the fusion of academic and private-practice advanced training programs. She has published scientific journal articles and textbook chapters on urinary diseases and other internal medicine topics, and speaks locally, nationally, and internationally on topics in nephrology and urology.
