I’ve got your back: Diagnosis and management of IVDD
Carolyn Nye, DVM
Massachusetts Veterinary Referral Hospital, Woburn, MA
Posted on 2017-07-18 in Neurology
Intervertebral disc disease (IVDD) is one of the most common neurological disorders of dogs and it is the most common spinal disease of dogs. This article discusses the definition of IVDD, presentation, diagnosis, management, and prognosis of dogs with intervertebral disc disease.
Definitions
Anatomy
The canine vertebral column is composed of 7 cervical, 13 thoracic, 7 lumbar, 3 fused sacral and 20 coccygeal vertebrae. There is an intervertebral disc located between each vertebra except for C1-C2 and the fused sacrum. These intervertebral discs sit between the vertebrae to allow for cushioning between bones as the animal runs, jumps and plays.
The intervertebral disc is composed of an inner jelly-like center called the nucleus pulposus and an outer fibrous casing called the annulus fibrosis. The weakest/thinnest part of the annulus is dorsal; so when a disc herniates it typically does so in the direction of the spinal cord, typically resulting in compressive and contusive injury to the cord.
Types of herniated discs
Hansen Type I disc ruptures are typically acute disc extrusions. They most commonly occur in chondrodystrophic (dwarf) breed dogs, in particular Dachshunds, French Bulldogs, Corgis and Basset Hounds. They result from a drying out of the nucleus pulposus, making the disc more prone to rupturing.
Hansen Type II discs are chronic bulging discs. These are typically seen in larger breed dogs. They typically result in chronic, progressive signs.
Hansen Type III discs are sometimes referred to as “missile discs”, “traumatic disc” or “low volume, high velocity”. These are non-surgical and result from the liquid nucleus pulposus hitting the spinal cord at high impact. There is no resulting compression as the material dissipates, but the cord experiences contusive injury.
Presentation
There are four clinical divisions of the spinal cord: C1-C5, C6-T2, T3-L3, and L4-S1(3). The presenting complaint and clinical signs depend on the area affected.
For a dog with a herniated disc, the presenting complaint typically ranges from back or neck pain to unable to walk.
When taking a history, there are many important questions to ask including the following:
- When were clinical signs first appreciated?
- Since initially seeing signs, have they progressed, stayed the same or improved?
- Does the owner think the pet is painful or just dysfunctional?
- Is the pet on any medications?
- Any previous history of back/neck pain or dysfunction?
Neurologic exam
The goal of the neurologic exam is to localize the disorder to a specific region of the nervous system. The neurologic exam is divided into five main categories; mentation, gait, reflexes, general proprioception, and pain. For a dog with intervertebral disc disease, mentation and cranial nerves should be normal. The gait is described first as ambulatory or non-ambulatory, followed by the limbs affected (mono-, para-, hemi-, or tetra-) then the suffix -paresis (weakness) or -plegia (paralysis).
Evaluation of gait helps you narrow down your localization either C1-T2 (if all limbs are affected) or T3-S2 (if only the hind limbs are affected.
So how do we narrow it down further?
Reflexes
A reflex arc is composed of a sensory nerve, a spinal cord segment, and a motor nerve. It DOES NOT NEED THE BRAIN – this is why you pull your hand away from the stove before even thinking, “that’s hot!”
The most reliable reflexes in dogs are withdrawal reflex (all limbs) and patellar reflex (pelvic limbs) C6-T2 contains the spinal segments responsible for reflexes in the forelimbs. L4-S2 contains the spinal segments responsible for reflexes in the pelvic limbs
Additional tests to help localize include palpating the spinal column to assess for pain and the cutaneous trunci.
With the addition of this information, you can localize to C1-C5, C6-T2, T3-L3 or L4-S2
The most common site of herniation in the back is T12-T13 (most commonly seen as Hansen type I disc in a small breed dog). The most common site in the neck in a small dog is C2-C3, and a large dog is C6-C7. It is rare for a disc to herniate in the cranial-mid thorax as the intra-capital ligament adds extra support in this area.
NOW WHAT? Differentials
Based on a neurologic exam we can tell WHERE The problem is, but not WHAT
Based on a combination of history and exam, we can make a list of reasonable differentials
- IVDD: can be any breed, but chondrodystrophic more common, usually young adult or older, usually painful (not always)
- Neoplasia: usually older, +/- painful, progressive
- Infection/inflammation: any age or breed, but most commonly young-adult small breed dogs (maltese, yorkie)
- FCEM (fibrocartilaginous embolic myelopathy): non-painful, non-progressive. Typically, young adult or older. Think of the lab who jumped up to catch a Frisbee, yelped, landed and was not able to walk.
- Acute non-compressive nucleus pulposus extrusion (ANNPE; “traumatic disc herniation,” Type III IVDD)
- Trauma: history of trauma, acute, painful
So… you have a dog that presents to your hospital and you are concerned it has disc disease
Neurologic grade
There are several different grading systems, one the more common is shown below:
- Grade 1: Pain only
- Grade 2: Ambulatory paretic
- Grade 3: Non-ambulatory paraparetic
- Grade 4: Paralyzed with intact nociception
- Grade 5: Paralyzed with absent nociception
Nonambulatory paraparetic (L>R) Coton de Tulear with an L3-4 disc extrusion.
When do you refer to a neurologist?
Referral is recommended when animals are minimally ambulatory or worse, there is rapid progression of clinical signs, there is failure to respond to medical management, or when you suspect the patient has something other than IVDD.
Treatment options: surgical vs medical
Medical management
Option for patients with back pain or minimal deficits that you strongly suspect has IVDD. Treatment based on presumptive diagnosis.
Diagnostics: CBC/biochemical profile/urinalysis. Unlikely to show a reason for underlying disease, however useful for selection of medications (NSAID) and to rule out other causes of “back pain,” such as acute renal failure.
Spinal radiographs? The only diseases that we can reliably diagnose on radiographs are discospondylitis (infection of the intervertebral disc and adjacent vertebral end plates), neoplasia causing a lytic lesion, and traumatic injuries (fracture/luxation). Failure to identify radiographic signs of discospondylitis or lytic bone lesion does not rule out these conditions and they are often more readily detected on MRI.
Radiographs can show signs of intervertebral disc disease, including narrowing/wedging of the intervertebral disc space, smaller intervertebral foramen size, narrowing of the articular process joint space, or mineralized disc material within the vertebral canal. However, these changes do not necessarily correlate to the primary lesion location.
While it is never wrong to obtain radiographs, especially if a referral is not allowed, they often do not provide enough specific information to make the diagnosis.
Pain medications
Gabapentin is our medication of choice for neuropathic pain. Tramadol can be used; however, its absorption and metabolism are inconsistent and we find it variable in efficacy. For chronic pain where owners are not interested in a referral, amantadine can be added.
Steroid vs NSAID
There is no proven benefit of steroids over NSAIDs in the literature. However, if an animal is on an NSAID and is getting worse, we like the option of starting it on a steroid. Empirically, we have had better success with steroids than NSAIDs, especially if the patient demonstrates weakness or ataxia. Exceptions are dogs with pain only where we suspect discospondylitis; these dogs we would consider an NSAID.
- Side effects of NSAIDs: potential for kidney and liver damage, GI ulceration, etc.
- Side effects of short course of steroid: polyphagia, polydipsia, polyuria, and sometimes panting, uncommon GI signs (nausea, vomiting, diarrhea, GI ulcers)
STRICT CRATE REST
In our opinion, this is THE MOST IMPORTANT aspect of medical management. We recommend a minimum of 2 weeks of strict rest involving crate confinement (or small confined space) at all times unless the patient is sitting quietly in the owner’s lap or right next to them, short controlled leash walks just long enough to urinate/defecate, and no running, jumping, or use of stairs. If normal the patient returns to normal at 2 weeks, we recommend a total of 4 weeks of strict rest before gradual return to activity. Referral is recommended if the patient worsens at any time.
Surgical management
When is surgical intervention recommended? When animals are minimally ambulatory or worse, or they have failed conservative management (gotten worse or failed to improve).
Diagnostics are dependent on age. CBC/biochemical profile/urinalysis and thoracic radiographs are considered in middle-aged to older patients. In young, otherwise healthy patients a PCV/TS/NOVA (mini-chem) is often sufficient.
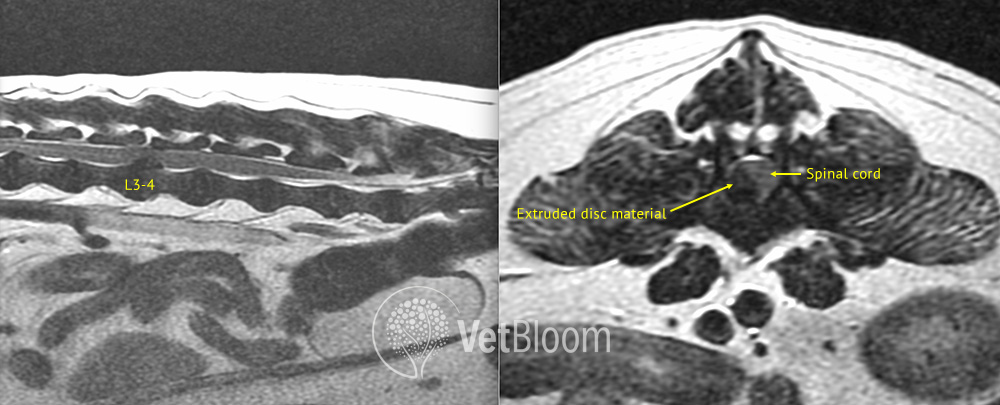
Right-sided L3-4 intervertebral disc extrusion causing significant spinal cord compression. Image courtesy of Mark Troxel, DVM, DACVIM (Neurology).
Advanced imaging is needed for definitive diagnosis and surgical planning. MRI is the gold standard (fig. 1); however, myelogram alone, CT alone, or CT/myelogram is acceptable under specific circumstances.
The MRI allows you to see soft tissue of the spinal cord, discs, and nerve roots, whether there is a herniated disc, and can assess for neoplasia, infection/inflammation, FCEM, and other conditions.
Surgery
The surgical procedure chosen depends on location. In general, a ventral slot surgery is performed most commonly in the neck because the disc material is most commonly located in the ventral or ventrolateral vertebral canal. A cervical dorsal laminectomy or hemilaminectomy is sometimes required if the disc material and/or blood clots is located laterally or extends dorsally around the cord. A hemilaminectomy is performed most commonly in the thoracic and lumbar regions.
Prognosis
The prognosis for animals with IVDD is generally good. Medical management carries a 60-75% chance for recovery even in patients that are paraplegic with intact nociception. Surgery carries an 85-95% chance for return to walking as long as the patient retains conscious perception of pain. If the patient has absent nociception, the prognosis for return to walking is 50/50 following surgery if pain was lost in the previous 24-48 hours.
Recurrence: The chance of recurrence at other sites is around 20%.
Down dog care – Considerations and tips
For both medically managed and surgically managed cases, a period of about 4 weeks of strict rest is necessary.
Managing a down dog
- Rotating the hips several times daily and monitoring for pressure sores. Patients should be kept on thick, soft bedding that gives support, but should offer some support.
- A sling is recommended, such as a “Help Em Up” harness. We prefer not a sling under the abdomen because it puts pressure on the caudal abdomen and can cause discomfort.
- Patients should be thought of as being “on bed rest” — 23.5 hours a day in the crate; other 30 minutes divided into 3-4 bathroom outings; outside, urinate/defecate, back to area of rest. Should be brought outside ON LEASH and using a sling support if needed. Avoid stairs.
- If patient is on prednisone, they will drink and urinate more. Can consider giving them an “ice brick” at night to slow them down.
- Physical therapy can be helpful. At home physical therapy includes supported standing and passive range of motion. Professional therapy that can be useful includes hydrotherapy and laser therapy.
Bladder care
Bladder management is very important for “down dogs”. Oftentimes, when dogs loose voluntary motor in their hind limbs, they lose the ability to urinate voluntarily. This can become a medical emergency. It is important to ask about recent urinations. If a dog is paralyzed, it is important to discuss bladder care. If the animal does not urinate for 24 hours, the owner needs to be taught either how to manually express the bladder or (if a male dog) pass a urinary catheter 2-3 times daily.
Long term management
Most dogs will recover. For those that don’t, wheelchairs are an option. Remember that while some owners will consider a wheel-chair pet, many do not take into account bladder management.
Even dogs that fully recover should have permanent lifestyle changes, including minimizing stairs, jumping on/off furniture, and rough play with other dogs. It is not possible to prevent recurrence (can happen in a crate) however we can minimize the risk.
Further reading
- De Lahunta, Glass, Kent. (2015). Veterinary Neuroanatomy and Clinical Neurology. MO, Saunders.
- Dewey, C.W., da Costa, R. C. (2016). Practical Guide to Canine and Feline Neurology. Ames, Iowa: John Wiley & Sons.
- Dhupa S, Glickman N, Waters DJ. Reoperative neurosurgery in dogs with thoracolumbar disc disease. Vet Surg 1999;28:421-8.
- Mann FA, Wagner-Mann CC, Dumphy ED et al. Recurrence rate of presumed thoracolumbar intervertebral disc disease in ambulatory dogs with spinal hyperpathia treated with anti-inflammatory drugs: 78 cases (1997-2000). J Vet Emerg Crit Care 2007;17:53-60.
About the author
|

 Dr. Nye graduated from Bates College with a bachelor of science in neuroscience before going to veterinary school. She was valedictorian of her class at St. Georges School of Veterinary Medicine in Grenada, West Indies where she received awards in pharmacology, internal medicine, large animal surgery, research and a peer nominated outstanding colleague award. She completed her final year of veterinary school at North Carolina State University, College of Veterinary Medicine, where she was presented with the award for proficiency in neurology. She performed research with their Neurology Service investigating the role of lactate in the CSF of patients with various neurologic conditions. After graduation she returned NCSU to work in the Emergency Department and to continue research. She then completed a rotating internship at Red Bank Veterinary Hospital in Tinton Falls, NJ and then a neurology specialty internship at Massachusetts Veterinary Referral Hospital. She is currently in a neurology & neurosurgery residency at The Ohio State University.
Dr. Nye graduated from Bates College with a bachelor of science in neuroscience before going to veterinary school. She was valedictorian of her class at St. Georges School of Veterinary Medicine in Grenada, West Indies where she received awards in pharmacology, internal medicine, large animal surgery, research and a peer nominated outstanding colleague award. She completed her final year of veterinary school at North Carolina State University, College of Veterinary Medicine, where she was presented with the award for proficiency in neurology. She performed research with their Neurology Service investigating the role of lactate in the CSF of patients with various neurologic conditions. After graduation she returned NCSU to work in the Emergency Department and to continue research. She then completed a rotating internship at Red Bank Veterinary Hospital in Tinton Falls, NJ and then a neurology specialty internship at Massachusetts Veterinary Referral Hospital. She is currently in a neurology & neurosurgery residency at The Ohio State University.
