Cranky kitties: Diagnosis and management of feline osteoarthritis
Lisa B. Corti, DVM, DACVS, CCRP
Massachusetts Veterinary Referral Hospital, Woburn, MA
Posted on 2017-02-28 in Surgery
Canine osteoarthritis (OA) is a well characterized chronic disease, with causes, clinical signs, radiographic abnormalities, and treatments well established. The same, however, cannot be said for feline osteoarthritis. Surprisingly little is still known about feline degenerative joint disease (DJD).1 DJD refers to the chronic progressive destruction of the components of synovial and cartilaginous joints, while OA refers to the inflammation of the joint and subchondral bone, as a result of DJD.1,3,4 The primary goals for these proceedings are to understand the differences between OA in dogs and cats, to recognize the clinical signs of OA in cats, and to be comfortable treating feline OA, including prescribing NSAIDs.
Causes for Osteoarthritis
Causes for OA in dogs are well known. Little evidence exists for the causes of OA in cats, and most of what is presented is speculation.1 Godfrey considered 89% of 292 cats with radiographic evidence of DJD to have primary DJD.2 Primary DJD occurs without any underlying cause. It is believed that the articular cartilage simply degenerates because of aging. Secondary DJD, or DJD that arises from an underlying condition, is very common in dogs. It includes congenital malformations, such as hip dysplasia and osteochondrosis, infectious and immune-mediated arthropathies, and metabolic disease such as obesity. It is suggested that because feline DJD is frequently bilateral, it probably does occur secondary to conditions similar to dogs.1,2,6 Cats can also develop OA secondary to hypervitaminosis A from a diet consisting predominantly of liver.1,3
Clinical Signs of Osteoarthritis
The most common clinical sign observed in dogs with appendicular OA is lameness. Usually, the lameness is unilateral, even though the OA is often bilateral. Dogs may also be slow and stiff after rest, may have difficulty rising or laying down, may have a decreased tolerance for exercise, a reluctance to jump, or reluctance to go up or down stairs. Physical exam findings are often consistent with a unilateral lameness, short-strided gait pattern, and muscle atrophy of the affected limb. Joint pain is usually elicited with decreased range of motion and joint effusion.
Clinical signs of OA in cats are vague and nonspecific.1,5,6,7,8 This is probably why, to this date, not much is known about OA in cats. Owners may report the following as signs of pain due to OA in their cats: a change in ability to jump up or down, not moving as smoothly up or down stairs, ill-tempered behavior, avoiding human interaction, seeking seclusion, sleeping more or less, not playing as much with toys or other pets in the household, a decrease in grooming behavior, difficulty stretching, not sharpening claws as often, and difficulty climbing in and out of the litter box, which may lead to constipation and soiling outside of the litter box. An astute observer will notice that this list does not include lameness. One study revealed that while 71% of cats with DJD showed changes in behavior, only 17% showed signs of lameness.6 OA pain in cats more commonly leads to a decrease in overall mobility and mood. If lameness is present, then the joint disease is usually fairly advanced.16 For both dogs and cats, however, any deviation from normal behavior can be a sign of pain and should not be overlooked.
Physical exams in cats can be challenging in and of themselves. Orthopedic exams on painful, cranky, kitties are especially challenging. Observing the cat from a distance—how he exits from the carrier, how he walks around the room, what his gait looks like, how he interacts with the exam room, does he show interest in jumping onto the furniture but hesitates, how he sits or lays down—sometimes gives you all the information you need. Because cats do not often exhibit a lameness, it becomes more important to palpate every limb and every joint, including the lumbosacral (L-S) area, for pain and instability. Some cats, however, will just not tolerate this. In dogs, I almost always evaluate the unaffected contralateral limb before examining the affected one. In cats, however, I will evaluate the limb that I suspect to be problematic first because sometimes that is the only chance I get for a hands-on exam. Some evidence suggests that orthopedic exam findings in cats are not reliable.9 Owners can be asked to video their cat at home at the time they make the appointment and bring the video with them to the exam. It is important to perform a neurologic exam, especially of the hind limbs, as many cats with L-S DJD have neurologic deficits to their hind limbs and tail.6 Detailed clinical recommendations for orthopedic and neurologic exams can be found elsewhere.16
Radiographic Evidence and Appearance of DJD
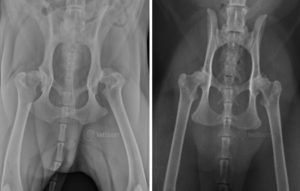
The prevalence of radiographic DJD in cats appears to be as high as it is in dogs, and also appears to increase with age. The prevalence in cats ranges from 22 to 90%,8 while one study found that 93 out of 100 randomly selected cats had radiographic evidence of DJD.9 All studies so far that have looked at radiographic evidence of DJD in cats have been retrospective, and so the populations of cats studied were not randomly selected. Most radiographs evaluated for these studies were those of the thorax, as it appears that cats are often radiographed for evaluation of their cardiopulmonary systems. The true prevalence, therefore, of DJD in cats is still unknown. Having said that, the appendicular joints most commonly reported to be affected with DJD in cats appear to be the elbow (fig. 1) and hip (fig. 2). The areas of the axial skeleton most commonly affected appear to be from the 7th to the 10th thoracic vertebrae, with the L-S joint displaying the most severe radiographic DJD of the axial skeleton.1,2,3,6
The radiographic appearance of DJD in cats differs somewhat from that of dogs. In DJD of dogs, we see thickening of peri-articular tissues, increased joint effusion, sclerosis of subchondral bone, and osteophyte and enthesiophyte formation. Thickening of the peri-articular tissues and an increase in joint fluid are not as common in cats,1,3 and feline DJD may be associated with a lower tendency for new bone formation.1 Intra-articular mineralizations occur more commonly in cats, as do subchondral bone cysts.3,6 Meniscal calcifications often appear in feline stifle radiographs (fig. 3) and may be an incidental finding or associated with cranial cruciate ligament rupture.1,3
Radiographs of feline coxofemoral DJD vary greatly from that of dogs. Anatomically, cats have a shallower acetabulum than dogs, with a mean Norberg angle (NA) of about 92o for cats and 103o for dogs.3 In addition, cats with a Distraction Index (DI) of less than 0.4 do not develop signs of DJD, while for dogs it is less than a DI of 0.3 that they are safe from DJD.3 This means that cats tolerate a looser hip joint than dogs, representing their superior flexibility and agility. With coxofemoral DJD in cats, most bony remodeling and proliferative changes appear on the craniodorsal acetabular rim in the ventrodorsal radiograph projection, and there is minimal remodeling of the femoral head and neck.3 This is in sharp contrast to the appearance of canine coxofemoral DJD, where there is significant remodeling of the femoral head and neck and global acetabular changes.
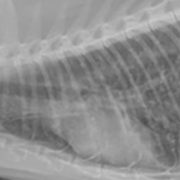
DJD of the L-S region in cats (fig. 4) looks similar to that of dogs, with narrowing of the disc space, vertebral endplate sclerosis, and lateral and ventral enthesiophyte formation.1,3 It is important to mention that when we see radiographic changes consistent with DJD in dogs, there is significant, and often advanced, cartilage degeneration present. We still cannot correlate radiographic DJD with histologic DJD in cats, as these studies have not been done. Essentially, we do not know how damaged or degenerated the cartilage is in cats based on the presence, or absence, of radiographic abnormalities. It is also important to note that, just as with dogs, radiographic DJD does not always correlate with orthopedic exam findings in cats.10

Fig. 4: Lateral radiographs obtained from a cat with an L7-S1 intervertebral disc protrusion (diagnosed on MRI) and stifle OA.
Minimum Database
In addition to radiographs, all cats presenting with OA should have a complete blood count, full chemistry panel, urinalysis, and urine culture submitted. A resting blood pressure may also be considered if renal disease is suspected. Geriatric cats should also have thoracic radiographs and an abdominal ultrasound performed. It is important to rule-out any underlying illnesses, including renal disease, in all age groups of cats, important to stabilize any illnesses before starting treatment for OA, and important for having longevity discussions with owners of geriatric patients.
Prevalence of Chronic Kidney Disease (CKD) in Cats
Any discussion of treatment for feline OA must include a discussion of renal disease because of the concern regarding the use of NSAIDs in cats and the potential effects NSAIDs have on the kidneys. Marino et.al. evaluated a randomly selected (RS) population of cats from ages 6 months to 20 years, and a group of cats recruited for DJD studies. Cats were evaluated for the presence of CKD based on the International Renal Interest Society (IRIS) staging system. Of the RS cats, half were CKD positive, with 33% of these in IRIS stage 2 kidney disease. Of the DJD cats, 68% were positive for CKD, with 45% deemed to be in stage 2 kidney disease. Researchers concluded that the prevalence of CKD was higher than expected in the general population, that cats of all ages should be screened for CKD, and there is a strong concurrence between DJD and CKD, with further research needed into whether there is a shared etiology between the two.10
Management of Feline Osteoarthritis
Just as with dogs, medical management of feline OA should be multimodal, incorporating the use of pharmaceuticals, changes in nutrition, and alterations to the home environment. A multimodal approach has been shown to provide the most effective pain relief from OA in both humans and animals. Surgical management of appendicular OA in cats is rarely necessary, and will not be discussed here.
There is no doubt that cats with OA are painful. Several studies out of North Carolina State University clearly demonstrate that when cats with OA are given an NSAID (specifically, meloxicam), their activity, mobility, mood, and quality of life all improve.1,4,7,8 Currently, there are no medications approved for the relief of pain due to OA in cats in the United States. In addition, there are no NSAIDs in the United States approved for long-term use in cats.14 Meloxicam is currently only FDA approved in cats for the control of postoperative pain associated with orthopedic surgery, ovariohysterectomy, and castration, and as a single subcutaneous dose. While oral meloxicam is used routinely in cats overseas, the FDA issued a warning statement in 2010 regarding the occurrence of acute renal failure with repeated use of injectable or oral meloxicam, stating that there is “no safe and effective dose of the oral suspension…approved for cats.”11 The FDA does concede that some veterinarians prescribe meloxicam in an extra-label manner and have the legal right to do so.11
So why is there this discrepancy between the United States and the international veterinary community regarding the use of oral meloxicam in cats? Recent studies may shed light on the answer to this query. One such study was a multi-center analysis of the long-term effects of meloxicam on renal function in cats with altered mobility due to DJD.12 All cats were older than 7 years and had received meloxicam for variable amounts of time in excess of 6 months. Cats were divided into two groups, those with CKD (renal group) and those without KD (non-renal group). Twenty-two cats had stable, mostly IRIS stage 2, CKD, and this renal group was treated with meloxicam for a median of 467 days. Sixteen cats were in the non-renal group and were treated for a median of 327 days. A group of control matched cats—22 for the renal group and 16 for the non-renal group—that were not treated with meloxicam were followed as well. Researchers found that meloxicam did not have any negative impact on renal function in cats with or without CKD. In fact, creatinine concentrations increased more slowly over time in the renal group treated with meloxicam than in the control cats not receiving meloxicam. In other words, meloxicam therapy seemed to have a beneficial effect in cats with CKD. There was also no significant difference in creatinine concentrations between the non-renal group treated with meloxicam, and the control matched cats not treated with meloxicam. Urine specific gravity decreased over time in all cats, and there was no significant difference found between the non-renal group treated with meloxicam and the control matched cats not treated with meloxicam.12 Clinically speaking, therefore, long-term meloxicam administration did not harm the kidneys of cats with DJD.
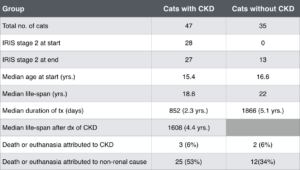
Table 1: Comparison of the longevity of cats with and without CKD treated with meloxicam. Modified from: Gowan R.A., et.al. A retrospective analysis of the effects of meloxicam on the longevity of aged cats with and without overt chronic kidney disease. Journal of Feline Medicine and Surgery (2012) 14, 876-881.
The starting dose of meloxicam in this study was 0.05 mg/kg SID. A week or two later, and every 3 to 6 months, the owners were contacted. If the cats were perceived to be improving, the dose of meloxicam was reduced. The median maintenance dose of meloxicam for the duration of the study was 0.02 mg/kg SID, with some cats receiving 0.1 mg or 2 drops of the 1.5 mg/ml oral suspension.12 The author of this study continued to follow this same group of cats, while including others for a total of 82 cats, until their deaths (Table 1).13 Forty-seven cats had CKD and 35 did not. Each group received a median meloxicam dose of 0.02 mg/kg SID for longer than 6 months. A summary comparison of the two groups is tabulated below.
“Long-term treatment with oral meloxicam,” therefore, “did not appear to reduce the lifespan of cats with pre-existent stable CKD.”13 Researchers concluded that meloxicam should be a part of the therapeutic regimen for cats with chronic painful conditions. Interestingly, 28% of the cats were euthanized because of progression of their OA, and 93% of owners would trade longevity for an increased quality of life in their cats.13
To return to the original question—why this discrepancy between the U.S. and countries overseas—we must look at the dose of meloxicam prescribed. It is my opinion that veterinarians in this country are using too high a dose of meloxicam in cats, and are inappropriately following the guidelines for dogs. While the approved daily oral meloxicam dose for dogs in this country is 0.1 mg/kg, the above studies report a median daily dose of 0.02 mg/kg for cats, an 80% reduction in dosage. Other researchers—Lascelles and Robertson—recommend an oral dose and dosage interval of 0.05 mg/kg every other day.1 Clinicians may consider starting at a dose of 0.05 mg/kg SID in cats and then titrating down to the lowest effective dose and dosing interval.
Robenacoxib is a newer NSAID approved in the U.S. for controlling postoperative pain in cats after orthopedic surgery, ovariohysterectomy, and castration for up to 3 days. King et.al. looked at the clinical safety of robenacoxib in 194 cats with OA treated for 28 days.14 Cats ranged in age from 8 months to 20 years, with a median of 15 years. Ninety-five cats received robenacoxib and 99 a placebo, with a subgroup of 40 cats diagnosed with concurrent CKD. Physical exam findings, body weight, blood work and urinalysis results, adverse events, and answers to owner questionnaires were recorded over time. No significant difference existed in the adverse event rates reported for robenacoxib and placebo, with fewer serious adverse events reported for robenacoxib. More importantly, there was no significant difference in body weight change reported for either treatment group, and there were no changes in hematologic, serum chemistry, or urine variables for either treatment group, including the cats with concurrent CKD at the start of the study. Cats, therefore, tolerated robenacoxib when it was given to them every day for a month, and there was no clinical indication of damage to the gastrointestinal tract, liver, or kidney, even in cats with CKD.14
In addition to prescribing either meloxicam or robenacoxib, feeding a diet rich in long-chain omega-3 fatty acids, specifically eicosapentaenoic (EPA) and docosahexaenoic acid (DHA), green-lipped mussel extract, and glucosamine/chondroitin sulfate may alleviate the pain associated with OA in cats. Forty cats, with decreases in activity and mobility attributed to their DJD, were randomly assigned to be fed either a test diet, containing the above-listed ingredients, or a control diet.9 The cats were evaluated on day 0, and again on days 14, 42, and 70. Client-specific outcome measures, activity monitor counts, orthopedic exam pain scores, activity visual analog scores, global quality of life, fecal scores, palatability scores, and blood and urine variables were recorded. The results indicated that cats fed the test diet had significant increases in their activities, increases in appetite, and decreased the amount of time spent sleeping, while cats fed the control diet had decreases in activities recorded over the study period. Dietary modification, therefore, may be a method to improve mobility in cats with DJD-associated pain,9 and if used in conjunction with an NSAID may allow the dose to be decreased.
Finally, providing enhancements and strategic alterations to a cat’s environment can help the patient overcome physical limitations and can improve overall physical and psychological well-being.15 Owners can facilitate access to heights, providing boxes, steps, or ramps for cats to climb. Patients should have easy access to the litter box, using a box with low sides and placing the box in plain site. Cats who do not groom themselves as often should be brushed regularly. More importantly, cats should be encouraged to exercise more, simulating their natural hunting behaviors. Daily moderate exercise decreases the pain and stiffness associated with OA, and can deter weight gain. This can take the form of dividing the patient’s meal into 3 or 4 smaller amounts and scattering them around the house; using a food toy (see video); scattering dry kibble all over the floor; or placing the cat’s water bowl in another room away from the food bowl. Interaction with feather wands, laser pointers, and catnip toys are also ways to encourage exercise and enhance the cat’s bond with the owner.
In general, I treat the pain associated with OA in cats with long-term meloxicam, starting at a daily dose of 0.05 mg/kg that decreases over time to the lowest effective dose, long-term gabapentin, starting at 10 mg/kg BID that slowly increases over time in both dose and frequency, Hill’s Feline J/D or Royal Canin Feline Senior Consult, and environmental modifications. I discuss physical rehabilitation at a certified facility, but some cats will not tolerate it, and many owners are reluctant to stress their cat driving to the hospital. As the disease progresses, I add amantadine 2-4 mg/kg BID or tramadol 4 mg/kg BID-TID, and often recommend acupuncture. I use Adequan in cats, but not frequently, and tend to not prescribe neutraceuticals as there is limited evidence to support their use, there are no regulations regarding their production, and they are expensive.
It is important to maintain close communication with these owners, and not lose follow up on these cats. Initially, I recommend rechecking blood work and UA’s, ortho and neuro exams, and body weight every 3 months if the cat is on regular NSAID therapy. If the cat has had stable CKD—has had stable renal values, stable appetite and body weight, negative urine cultures, etc.—I will recheck blood work and a UA 2-3 weeks after starting NSAID therapy, and then every 3 months thereafter. CKD will progress, but based on the best evidence we have, appears to do so regardless of NSAID therapy.
References
- Lascelles B.D.X. Feline Degenerative Joint Disease. Vet Surg 39:2-13, 2010.
- Godfrey D.R. Osteoarthritis in cats: a retrospective radiological study. JSAP (2005);46, 425-429.
- Allan G.S. Radiographs Features of Feline Joint Diseases. Vet Clinics North American: Sm An Practice 30, No. 2, March 2000:281-302.
- Lascelles B.D.X., et.al. Evaluation of Client-Specific Outcome Measures and Activity Monitoring to Measure Pain Relief in Cats with Osteoarthritis. J Vet Intern Med 2007;21:410-416.
- Hill’s Pet Nutrition, Inc. Update on evidence-based clinical nutrition. Hill’s Prescription Diet j/d Feline. Technical Information Services, 2009.
- Hardie E.M., Roe S.C., Martin F.R. Radiographic evidence of degenerative joint disease in geriatric cats: 100 cases (1994-1997). JAVMA, Vol. 220, No. 5, March 1, 2002.
- Benito J., et.al. Feline Musculoskeletal Pain Index: Responsiveness and Testing of Criterion Validity. J Vet Intern Med 2013;27:474-482.
- Gruen M.E., et.al. Detection of Clinically Relevant Pain Relief in Cats with Degenerative Joint Disease Associated Pain. J Vet Intern Med 2014;28:346-350.
- Lascelles B.D.X., et.al. Evaluation of a Therapeutic Diet for Feline Degenerative Joint Disease. J Vet Intern Med 2010;24:487-495.
- Marino C.L., et.al. Prevalence and classification of chronic kidney disease in cats randomly selected from four age groups and in cats recruited for degenerative joint disease studies. Journal of Feline Medicine and Surgery (2014) 16, 465-472.
- S. Food and Drug Administration CVM updates, FDA Announces Addition of Boxed Warning to Metacam® (meloxicam) Labels, www.fda.gov, October 27, 2010.
- Gowan R.A., et.al. Retrospective case-control study of the effects of long-term dosing with meloxicam on renal function in aged cats with degenerative joint disease. Journal of Feline Medicine and Surgery (2011) 13, 752-761.
- Gowan R.A., et.al. A retrospective analysis of the effects of meloxicam on the longevity of aged cats with and without overt chronic kidney disease. Journal of Feline Medicine and Surgery (2012) 14, 876-881.
- King J.N., et.al. Clinical safety of robenacoxib in feline osteoarthritis: results of a randomized, blinded, placebo-controlled clinical trial. Journal of Feline Medicine and Surgery (2015) 1-11.
- Bennett D., Ariffin S.M.bt.Z., Johnston P. Osteoarthritis In The Cat. 2.How should it be managed and treated? Journal of Feline Medicine and Surgery (2012) 14, 76-84.
- Kerwin S. Orthopedic Examination in the Cat. Clinical tips for ruling in/out common musculoskeletal disease. Journal of Feline Medicine and Surgery (2012) 14, 6-12.