Challenges in diagnosing lymphoid neoplasia
Carolyn Grimes, DVM, DACVP (Clinical Pathology)
STAT Veterinary Lab, Ethos Diagnostic Science, San Diego, CA
Posted on 2018-02-27 in Clinical Pathology & Oncology
The lymphatic system is a beautiful and infinitely complex network of cells, tissues, and organs designed to respond to diverse antigens that may present on almost every pathogen imaginable. The three major types of lymphocytes are T-cells, B-cells, and natural killer (NK) cells. Of these, T-cells and B-cells are the most frequently implicated in lymphoproliferative disorders. The ability of T-cells and B-cells to respond to such a diverse spectrum of antigens is attributed to the diversity of the antigen binding sites of their receptors. The receptors are each composed of a constant region that is common to all T-cell (or B-cell) receptors and a variable region. The variable region affords each cell its unique antigen specificity. It is produced through a special kind of genetic recombination that occurs during lymphocyte development.
When a lymphocyte encounters an antigen or antigen fragment that “fits” its receptor, it becomes activated. This triggers proliferation of the lymphocyte, producing a clonal population of cells that have the same receptor as its parent cell. Because most pathogens contain several antigens, they typically will activate many different B- and T- lymphocytes, resulting in several clonal proliferations (a polyclonal population). In contrast, when a lymphocyte undergoes neoplastic transformation and proliferates independent of pathogen activation and other cell regulatory mechanisms, a single clone proliferates to form a monoclonal population.
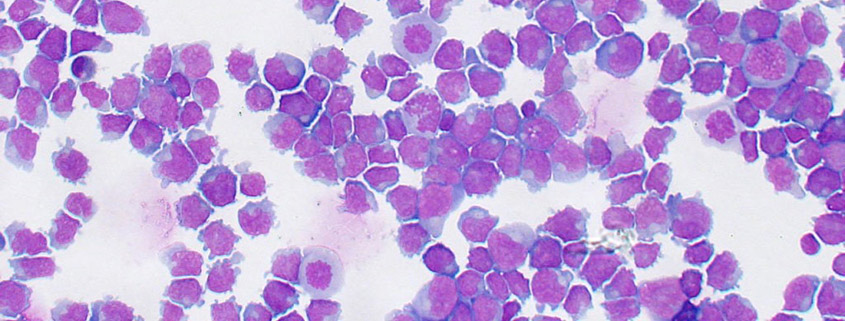
Distinguishing polyclonality from monoclonality is key when determining whether a lymphoid population is reactive or neoplastic. In many cases, identification of monoclonality by cytologic (lymphoma) or hematologic (lymphoid leukemia) examination is relatively straightforward. A benign population typically consists of mixed lymphoid cells, of which small lymphocytes predominate. A homogeneous population of large lymphocytes is therefore easily recognizable as neoplastic. There are, however, several situations in which distinguishing neoplastic from reactive proliferations is challenging. (1) In small cell lymphoma, the neoplastic cells appear very similar to small, non-neoplastic lymphocytes. Because small lymphocytes predominate in non-neoplastic (i.e., normal, inflamed, or reactive) lymphoid tissue, it can be difficult to determine whether “normal-looking” small lymphocytes are part of a benign or neoplastic population. (2) Emerging lymphoma poses a diagnostic challenge because, in many cases, the neoplastic cell population has not yet overtaken the benign (resident) population. In such cases, a mixed population is present and may appear reactive. (3) On a blood smear, when high numbers of large atypical lymphocytes are present, a diagnosis of lymphoid neoplasia may be obvious. However, when there are low numbers of circulating atypical lymphocytes, it is virtually impossible to determine whether they are part of a monoclonal or polyclonal population. (4) In the spleen, activated lymphoid follicles may contain high numbers of large lymphocytes. Aspirates from this tissue will contain high proportions of large lymphocytes that can be mistaken for neoplasia.
In such cases, additional testing such as flow cytometry or PARR (PCR for Antigen Receptor Rearrangement) may be necessary to confirm or exclude lymphoid neoplasia. Although PARR and flow cytometry have some overlapping uses, they have important differences that should be considered when deciding on which to use. PARR is truly a test of clonality; the conserved part of the receptor gene is detected by primers, then the remaining sequence is amplified by PCR. If a polyclonal population is present, multiple gene products (representing multiple different T-cell and B-cell receptors) are identified. In monoclonal populations, a single clone is detected. In flow cytometry, cellular components that serve as identifiers of a certain cell type (B-cell, helper T-cell, cytotoxic T-cell) are detected and quantified. Their relative quantities are used to determine if a population is mixed (benign) or homogeneous (neoplastic). Either flow or PARR are helpful in most cases. Flow has the advantage of providing phenotypic (e.g., lymphocyte subtype) data, which is often useful prognostically. However, when the lymphoid population is mixed (as may be the case in emerging lymphoma, low numbers of circulating atypical cells, and some splenic aspirates), flow cytometry may yield equivocal results and PARR is likely to be more helpful.
Distinguishing reactive from neoplastic lymphocytes is not always easy or straightforward. Recognizing the limitations of cytology and routine hematology is essential for understanding why a diagnosis cannot always be reached by these methods, when results should be questioned, and when additional tests should be pursued.
About the author
|

 Dr. Grimes earned her BS in biology from the University of Notre Dame in 2001, then her DVM at Purdue University in 2006. She completed a rotating internship in small animal medicine and surgery at Angell Animal Medical Center in Boston, MA in 2007, then practiced for two years as an emergency veterinarian for small animals at Red Bank Veterinary Hospital in New Jersey. She completed a residency in clinical pathology at the University of Tennessee in 2012, then joined the faculty of at the University of Montreal, where she worked in the clinical laboratory, taught in the veterinary curriculum, and did research that focused mainly on hematopathology and optimization of hematology analyzers.
Dr. Grimes earned her BS in biology from the University of Notre Dame in 2001, then her DVM at Purdue University in 2006. She completed a rotating internship in small animal medicine and surgery at Angell Animal Medical Center in Boston, MA in 2007, then practiced for two years as an emergency veterinarian for small animals at Red Bank Veterinary Hospital in New Jersey. She completed a residency in clinical pathology at the University of Tennessee in 2012, then joined the faculty of at the University of Montreal, where she worked in the clinical laboratory, taught in the veterinary curriculum, and did research that focused mainly on hematopathology and optimization of hematology analyzers.
